Maxillofacial surgery can be life-changing for patients dealing with severe facial injuries, congenital abnormalities, or dental issues that go beyond routine care. However, one significant concern for many considering these procedures is cost. Will your health insurance cover maxillofacial surgery, or will you need to foot the bill out of pocket?
This blog post will guide you through everything you need to know about insurance coverage for maxillofacial surgery. We’ll explore how insurance works, factors influencing coverage, common reasons for denied claims, and what steps you can take if your claim is rejected.
What Is Maxillofacial Surgery?
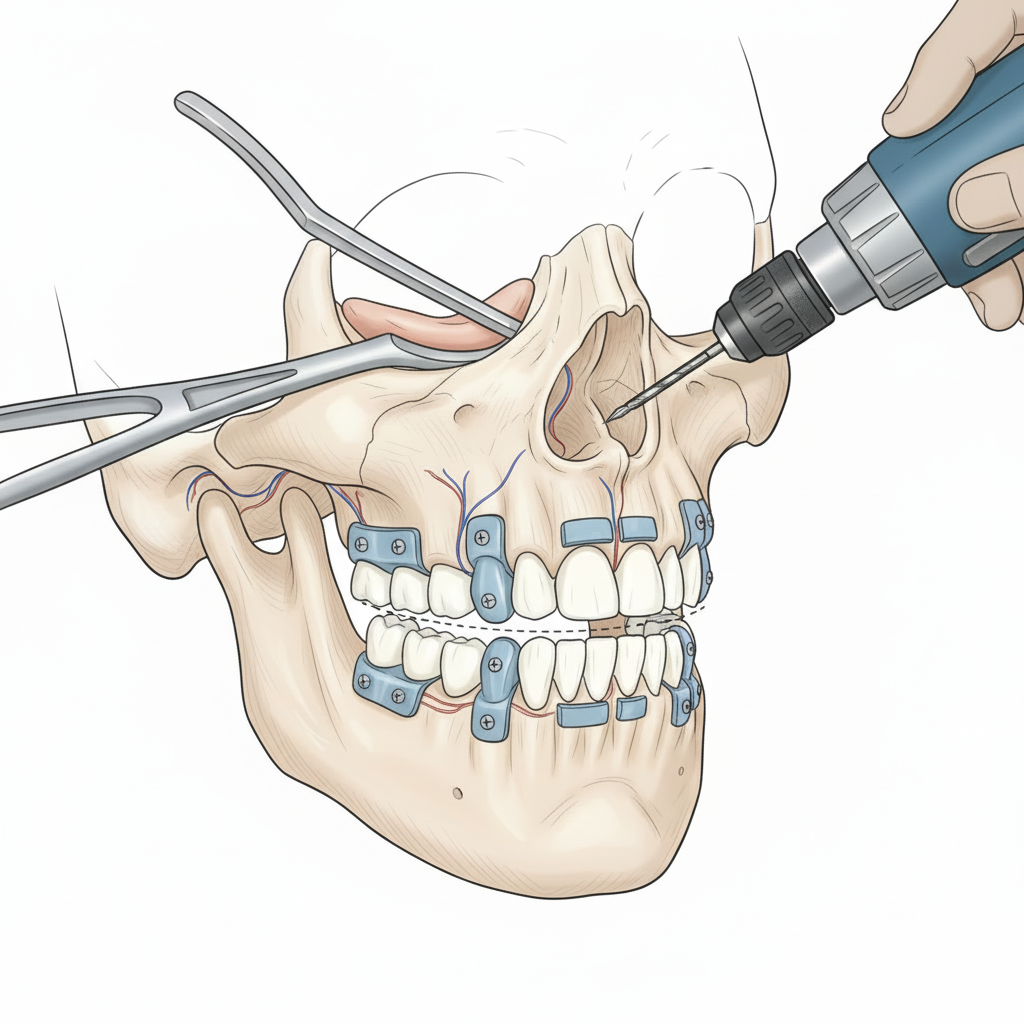
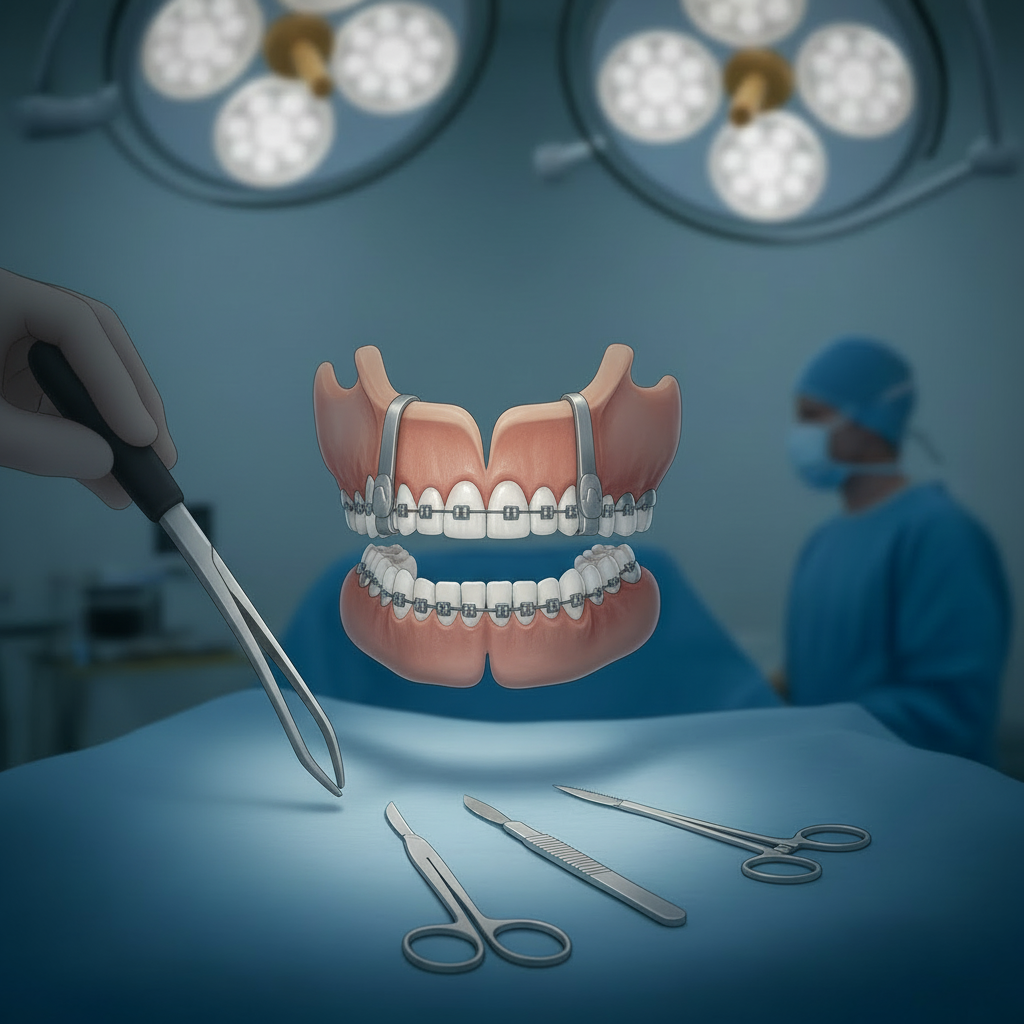
Maxillofacial surgery refers to medical procedures that focus on treating injuries or abnormalities of the face, jaw, mouth, and neck. It’s a specialized branch of surgery performed by oral and maxillofacial surgeons. These surgeries are often required for:
- Serious trauma or injuries to the facial area (e.g., fractures of the jaw or cheekbone)
- Disorders like temporomandibular joint (TMJ) dysfunction
- Oral cancers and tumor removals
- Cleft lip or palate reconstruction
- Severe dental issues, such as impacted wisdom teeth or dental implants linked to bone grafting
The cost of maxillofacial surgery can vary widely depending on the complexity of the procedure and the location. This makes insurance coverage an important factor in planning the treatment.
Understanding Health Insurance and How It Applies to Surgery
Broadly speaking, health insurance is designed to cover medical treatments deemed “medically necessary.” However, the definition of “medical necessity” can differ between insurance providers, and this ambiguity often causes confusion regarding maxillofacial surgery coverage.
When Insurance Typically Covers Surgery
Your health insurance is likely to cover maxillofacial surgery when:
- The surgery is required due to medical necessity (e.g., jaw fractures or tumors).
- It is part of reconstructive surgery following an accident or illness. For example, surgeries after facial trauma sustained in a car accident are usually covered.
- It’s tied to preventing further health issues. TMJ surgery or facial corrections that improve breathing and eating may be covered under these circumstances.
Dental vs. Medical Insurance
One key factor to note is whether the procedure falls under dental or medical insurance. Maxillofacial surgery often straddles the line between the two, and coverage depends on how the surgery is categorized. For example:
- Removing an impacted wisdom tooth may be considered a dental procedure.
- Surgery for a jaw injury resulting from an accident that affects your ability to eat or breathe may be deemed a medical procedure.
Understanding the difference can help you maneuver potential insurance hurdles.
Factors Affecting Insurance Coverage for Maxillofacial Surgery
Insurance coverage is not always straightforward. Several factors can determine whether your insurance policy will cover the cost of maxillofacial surgery.
1. Medical Necessity
Most health insurance plans require proof that the surgery is not elective or cosmetic. This means your doctor or surgeon must describe why the procedure is vital for your overall health in terms of functionality (e.g., improving breathing, reducing chronic pain).
2. Specific Policy Language
Each policy has unique terms and limits. While some health insurance plans explicitly cover maxillofacial surgeries, others may restrict or exclude coverage for certain procedures. Always read your policy details carefully, especially exclusions.
3. Pre-Approvals and Referrals
Many insurance companies require prior authorization for surgical procedures. This means your surgeon may need to submit documents explaining the medical necessity of the surgery in detail. Lack of prior approval can lead to claim denial.
4. Provider Network
Insurance providers often require patients to work with doctors and surgeons within their designated network. Going out-of-network may significantly reduce the reimbursement percentage or leave you responsible for paying entirely out of pocket.
Common Reasons for Coverage Denial
Even if the surgery seems medically necessary, coverage is not guaranteed. Here are a few common reasons why claims for maxillofacial surgery could be denied:
- Procedural confusion between dental and medical coverage.
- The insurance provider deems the surgery to be “cosmetic.”
- Missing or incomplete documentation for medical necessity.
- Using out-of-network surgeons or facilities.
- Failing to obtain pre-approval before surgery.
How to Appeal a Denial
A claim denial can be frustrating, but it doesn’t have to be the end of the road. Here are the steps you can take to file an appeal:
- Understand the Reason for Denial
Carefully review the denial letter to understand why your claim was rejected. Insurers are required to provide you with this information.
- Work With Your Surgeon
Maxillofacial surgeons are experienced in helping patients submit appeals. They can provide additional documentation or letters to substantiate the medical need for the surgery.
- Submit a Formal Appeal
Follow your insurer’s appeal process, which will likely involve submitting a written explanation along with medical records, imaging results, and professional recommendations.
- Use External Reviews
If your appeal is still denied, you may request an external review by an independent third party. This reviewer will assess whether the insurance decision adheres to the policy terms.
Alternative Payment Options
When insurance falls short or doesn’t cover your maxillofacial surgery, several alternatives can help manage costs:
- Payment Plans with Providers
Many surgeons and clinics offer payment plans to spread out the cost over time.
- Medical Loans
Some financial institutions and specialty lenders provide loans specifically for medical procedures.
- CareCredit
This healthcare credit card lets you pay for medical expenses, often with no-interest payment options.
- Health Savings Accounts (HSAs) or Flexible Spending Accounts (FSAs)
If you’re enrolled in an HSA or FSA program, you may be able to use this pre-tax money to cover qualified medical expenses.
- Charity Organizations
Consider reaching out to foundations and nonprofit organizations that assist patients in paying for surgeries.
Navigating Insurance for Maxillofacial Surgery
Maxillofacial surgery can play a critical role in restoring functionality and improving your quality of life—but navigating insurance for it can be complex. By understanding your policy, gathering strong documentation, and knowing your rights, you can improve your chances of getting the coverage you deserve.
Still unsure where to start? Speak with your healthcare provider or insurance company to get personalized guidance. A proactive approach will ensure you’re financially prepared and able to focus on what matters most: your recovery.