Hemifacial Microsomia – Congenital Deformed or Absent TMJ (Case 8)
Hemifacial microsomia (HFM) is one of the common congenital syndromes that can cause facial deformities.
Clinical and radiographic features of HFM usually include:
Unilateral hypoplasia or aplasia of the mandibular condyle, ramus, and body as well as hypoplasia of the maxilla, zygomatico-orbital complex, and temporal bone; decreased ipsilateral facial height; retruded mandible deviated towards the ipsilateral side; Class II malocclusion; transverse cant in the occlusal plane and skeletal structures; significant soft tissue deficiency on the involved side affecting muscles, subcutaneous tissues and skin volume, and decreased oropharyngeal airway.
With growth, the facial deformity, asymmetry, and malocclusion usually worsen.
Approximately 1/3 of the HFM cases will have displaced articular discs on the contralateral side.
These patients should be evaluated for this concomitant occurrence, and a TMJ MRI study will be warranted for the diagnosis. Our treatment protocol for managing HFM for patients 14 years or older who have significant hypoplasia or absence of the TMJ includes the following:
- Ipsilateral TMJ reconstruction, and mandibular advancement with custom-fitted total joint prostheses
- Contralateral disc repositioning with Mitek anchor
- Contralateral ramus sagittal split osteotomy to advance the mandible,
- Multiple maxillary osteotomies to transversely level, advance, and rotate counter-clockwise
- Fat graft to ipsilateral total joint prosthesis, and
- Ancillary procedures (i.e. Genioplasty, Rhinoplasty, Turbinectomies, etc.).
Surgery stage 2 for additional bony and soft tissue augmentation on the ipsilateral side. This protocol will provide the most stable and predictable treatment outcomes.
A patient with HFM who is 6 to 12 years old with absence of the TMJ may benefit from a growth center transplant using a sternoclavicular graft or rib graft. Rib grafts are unpredictable relative to growth and stability. Sternoclavicular grafts tend to have better growth potential, similar to normal TMJ growth.
Orthognathic surgery may be necessary at a later age (following completion of growth) to maximize the functional and aesthetic results.
Teenage or older patients with significant deformity of the condyle and ramus may have a much better outcome using a patient-fitted TMJ total joint prosthesis (TMJ Concepts system, to advance and lengthen the ramus on the ipsilateral side.
Deferring treatment until the patient is closer to completion of facial growth (girls, 15 years old; boys, 17–18 years old) helps minimize subsequent contralateral normal growth effect on the treatment outcome.
A mandibular ramus sagittal split osteotomy can be performed on the contralateral side, and the indicated maxillary osteotomies can be completed as well as any other adjunct procedures. Additional reconstruction may be necessary using bone grafts, synthetic bone, or alloplastic implants to build up the residual deformed skeletal structures.
Soft tissue reconstruction using fat grafts, tissue flaps, and vascularized free flaps, for example, may be necessary to fill out the soft tissue defects.
CASE 8. Hemifacial Microsomia (Figures 58 Through 60)
Figure 58:
(A-D) Patient is a 14-year-old female, diagnosed with Hemifacial microsomia. The left condyle and fossa were poorly developed, and patient developed worsening facial asymmetry over the years. The maxilla and mandible are retruded. The MRI evaluation of the right joint showed an anteriorly displaced disc and the cephalometric analysis signified a moderately constricted airway. Presurgery cephalometric evaluation and surgical treatment objective tracings were completed for the case to achieve the best aesthetic and functional outcome.
(E-H) The patient is seen 3 years postsurgery following single stage surgical procedures:
- Left mandibular TMJ reconstruction, mandibular advancement, and counterclockwise rotation with custom-fitted TMJ Concepts joint prosthesis;
- Repositioning of the right TMJ anteriorly displaced TMJ disc, using Mitek anchor;
- Right mandibular ramus osteotomy for advancement and counterclockwise rotation;
- Le Fort I osteotomy for maxillary advancement, down-grafting, and correction of maxillary occlusal plane discrepancy;
- Abdominal fat graft to the left TMJ, for prevention of heterotopic bone formation.
Figure 59:
A-C) The presurgery occlusion shows a left side posterior cross bite an transverse cant in the occlusal plane.
D-F) The occlusion is observed at 3 years postsurgery.
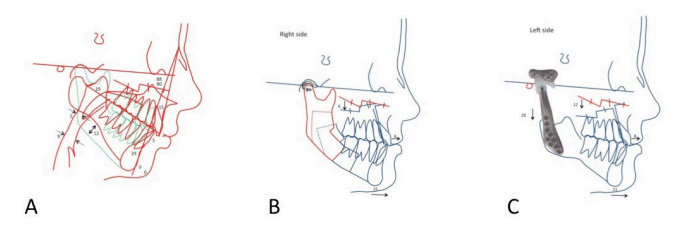
Figure 60:
A) Presurgery cephalometric analysis shows the retruded maxilla and mandible, high occlusal plane angle, and vertical asymmetry.
B) The surgical treatment objective for the right side demonstrates repositioning of the displaced TMJ disc, advancement of the mandible with a sagittal split osteotomy, and down-graft of the posterior maxilla and advancement.
C) The left TMJ and mandibular advancement is accomplished with the custom-fitted total joint prostheses, along with posterior down-graft of the maxilla (12 mm) and advancement, Pogonion advanced 21 mm.
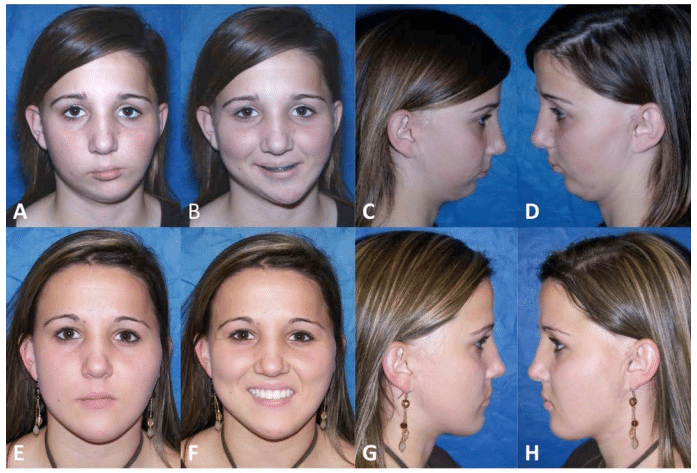
Figure 58, Case 8: (A-D) Presurgery clinical photos of a 14 year-old-female with left sided Hemifacial Microsomia, (E-H) Clinical photos, 3 years post surgery, at age 17.
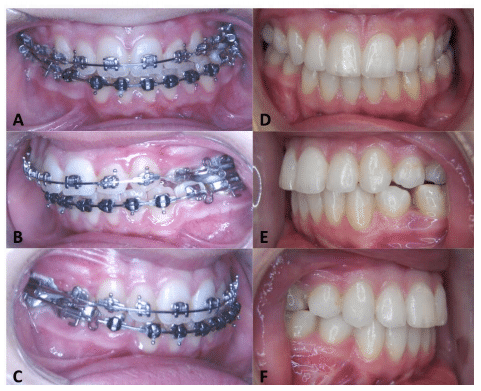
Figure 59, Case 8: (A-C) Presurgery and D-F) 3 year post surgery occlusal photos.
Figure 60, Case 9: A) Presurgery cephalometric evaluation, B) Surgical treatment objective of the right side, and C) the left side.