TMJ Ankylosis – Temporomandibular Joint Ankylosis
Case 7
Temporomandibular Joint bony ankylosis, TMJ Ankylosis, usually develops as a result of trauma, inflammation, sepsis, and/or systemic diseases causing severely limited jaw function as well as oral hygiene and nutritional problems. When this condition occurs during the growing years, it can severely affect jaw growth and development.
In unilateral ankylosis, the other condyle will continue to grow but may be retarded in its true growth potential. The common clinical and radiographic characteristics of TMJ ankylosis, particularly when occurring in children, include: Decreased jaw mobility and function; decreased growth on the involved side; facial asymmetry if unilateral involvement with the mandible shifted towards the ipsilateral side; retruded mandible; usually a Class II occlusion; and radiographic and MRI evidence of bony ankylosis between the condyle and the fossa or heterotopic bone surrounding the joint.
The most predictable treatment for the ankylosed TMJ patient includes:
- Release of the ankylosed joint; removal of the heterotopic and reactive bone with thorough debridement of the TMJ and adjacent areas;
- Reconstruct the TMJs (and if indicated, advance the mandible) with a custom-fitted total joint prosthesis;
- Coronoidotomies or coronoidectomies if the ramus is significantly advanced or vertically lengthened with the prosthesis;
- Autogenous fat graft (harvested from the abdomen or buttock) packed around the prosthesis in the TMJ area; and
- Additional orthognathic surgery if indicated. In these cases it is absolutely necessary that fat grafts be packed around the articulating parts of the prosthesis to prevent the reoccurrence of heterotopic and reactive bone as well as minimize fibrosis.
Other techniques that have been advocated for reconstruction of TMJ ankylosis include using autogenous tissues such as temporal fascia and muscle flaps, dermis-fat grafts, rib grafts, sternoclavicular grafts, vertical sliding osteotomy, gap arthroplasty, etc.
The total joint prosthesis with a fat graft packed around it is a superior technique relative to prevention of re-ankylosis, provide jaw and occlusion stability, improve function and facial balance, and eliminate or decrease pain. When treating young growing patients (10 years or older), the custom-fitted total joint prosthesis with fat graft may still be the best option to eliminate the TMJ ankylosis.
However, since there would be no growth potential on the ipsilateral side of the mandible (there is also no growth potential with a bony ankylosis), orthognathic surgery will likely be necessary, but can be delayed until the patient has most of the facial growth complete (females age 15 years, males age 17 to 18 years).
Then double jaw orthognathic surgery can be performed, including a ramus sagittal split on the side of the prosthesis to reposition the jaws into the best alignment, or the ipsilateral side can be advanced by repositioning the mandibular component of the prosthesis or fabrication of a new, longer mandibular component.
When a significant jaw deformity co-exists, It can be corrected at the same time with the following sequencing, done in a single surgical stage:
- Condylectomy, removal of heterotopic bone and fibrosis
- Coronoidotomy or coronoidectomy if indicated for more severe deformities requiring significant mandibular advancement or vertical lengthening
- If unilateral ankylosis, mandibular ramus osteotomy on the contralateral (opposite) side
- Mobilize mandible
- Maxillomandibular fixation with intermediate surgical splint
- Rigid fixation to contralateral mandibular ramus osteotomy
- Placement of total joint prostheses
- TMJ fat graft harvested from the abdomen or buttock packed around prosthesis
- Maxillary osteotomies and mobilization
- Turbinectomies, septoplasty, etc., if indicated
- Maxillary segmentation and application of the palatal splint if indicated
- Maxillary rigid fixation and bone grafting
- Adjunctive procedures such as genioplasty, rhinoplasty, UPPP, facial augmentation, etc.
Case 7. TMJ Ankylosis (Figures 56 AND 57)
Figure 56:
(A–D) A 15-year-old boy sustained mandibular trauma at age 8 years, resulting in (1) Right TMJ bony ankylosis and left TMJ fibrous ankylosis; (2) Retruded mandible and maxilla with high occlusal plane angle facial morphology; (3) Hypertrophied turbinates, adenoids, and tonsils; (4) Impacted third molars; and (5) Sleep apnea.
E-H) Patient seen 2 years postsurgery for the following procedures performed as a single stage surgery: (1) Bilateral TMJ reconstruction and mandibular counterclockwise advancement with custom-fitted TMJ Concepts total joint prostheses; (2) Maxillary osteotomies; (3) Turbinectomy, tonsillectomy, and adenoidectomy; (4) Removal of third molars; and (5) chin implant with pogonion advancing a total of 20 mm. At 2 years post surgery the patient was pain free, good skeletal and occlusal stability, good function, facial balance, and an incisal opening of 54 mm.
Figure 57:
A) Cephalometric tracing shows the retruded maxilla and mandible with high occlusal plane angle. The oropharyngeal airway is significantly decreased, hyperplastic adenoid tissue is present, and a Class II occlusion.
B) Surgical treatment objective tracing shows the advancement of the maxilla and mandible in a counterclockwise direction using TMJ Concepts total joint prostheses to reconstruct the TMJs and mandible as well as genioplasty with pogonion advancing a total of 20 mm.
C) Presurgery panogram shows the ankylosed right TMJ and evidence of attempted repair of the original right subcondylar fracture.
D) Post surgery radiographs show the bilateral TMJ Concepts total joint prostheses and bone plates securing the maxilla.
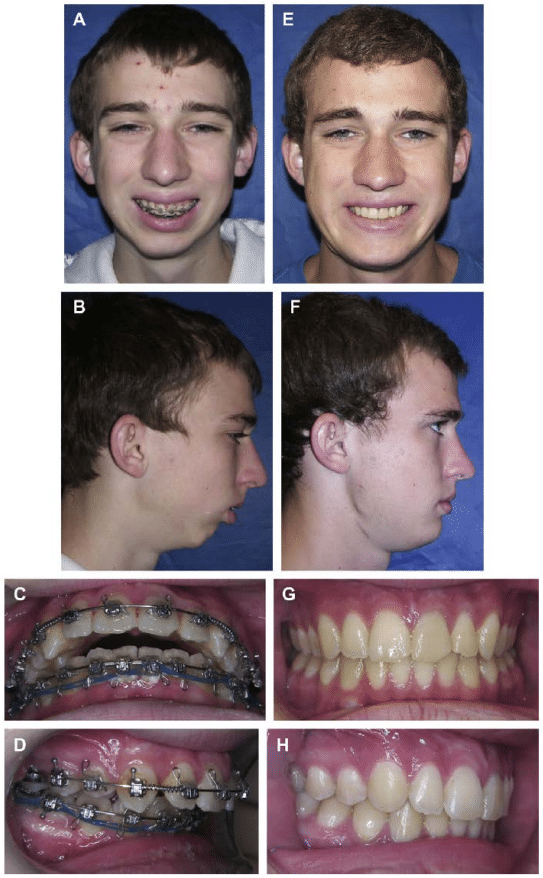
Figure 56, Case 7: A-D) Presurgery clinical and intraoral images, E-H) 2 year postsurgery clinical and occlusal photographs.
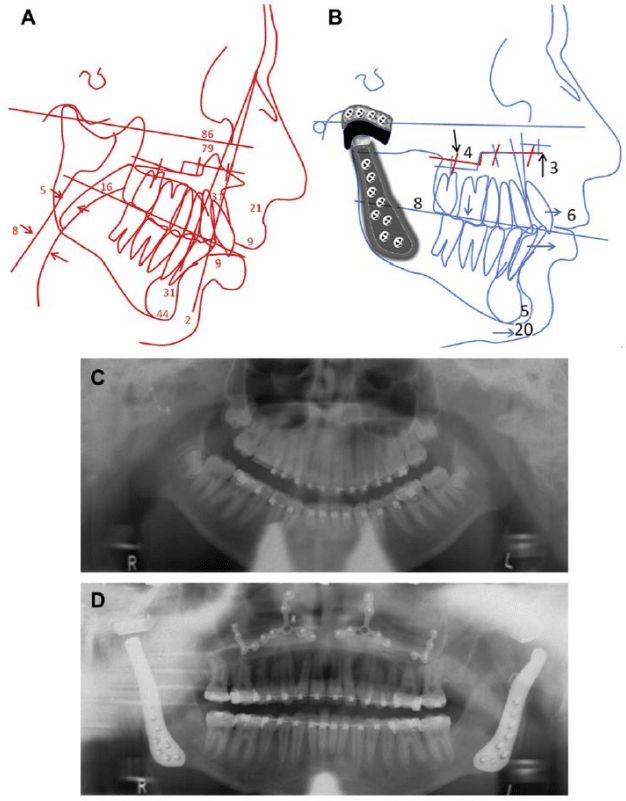
Figure 57, Case 7: A) Presurgery lateral cephalogram demonstrates the retruded maxilla and mandible as well as the high occlusal plane angulation. B) Surgical treatment objective tracing, C) presurgery panoramic x-ray, and D) postsurgery panoramic x-ray at 2 years.

