A comprehensive diagnostic list can be compiled following completion of all necessary and required evaluations.
Treatment Plan for TMJ Surgery
A definitive treatment plan for TMJ Surgery is developed to address these issues as well as other treatment options that may be available for the patient, so the patient can make an informed decision as to the treatment preferred.
The importance of disc position for stability cannot be overemphasized. Many surgeons have been thought that orthognathic surgery will “fix” the TMJ problems, however in patients with anteriorly displaced discs, particularly when mandibular advancement is required the articular disc remains anteriorly displaced with predictably increased pain and possibility of condylar resorption. Orthognathic surgery does not fix displaced discs.
Intraoperative Surgical Sequencing:
Intraoperative Surgical Sequencing for Disc Repositioning
Indicated surgical procedures are dependent of the TMJ condition and pathology as well as the severity of the jaw deformity. In some situations, the surgery may be much simpler than the following surgical sequencing protocol, which is designed for more complex Orthognathic Surgery in Combination with Disc Repositioning:
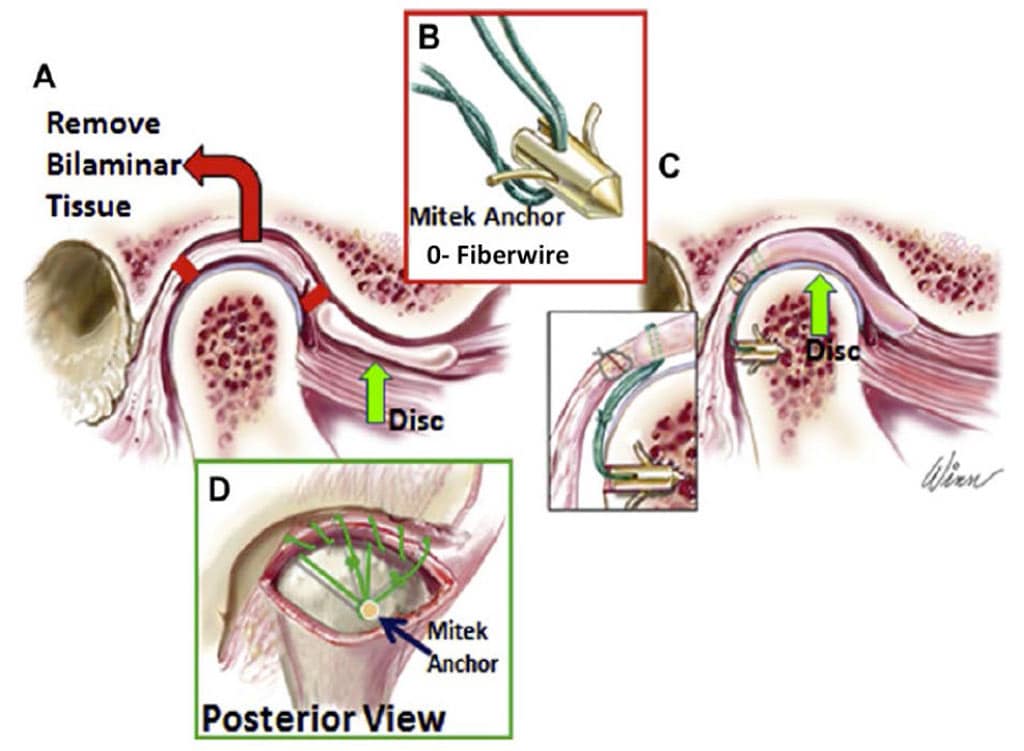
- TMJ disc repositioning with Mitek anchor and artificial ligaments
- Mandibular ramus osteotomies and mobilization
- Maxillomandibular fixation with intermediate surgical splint
- Placement of mandibular rigid fixation
- Maxillary osteotomies and mobilization
- Turbinectomies (partial), septoplasty, adenoidectomy etc., if indicated
- Maxillary segmentation and application of the palatal splint if indicated
- Maxillary positioning, rigid fixation and bone grafting
- Adjunctive procedures such as genioplasty, rhinoplasty, UPPP, facial augmentation, etc.
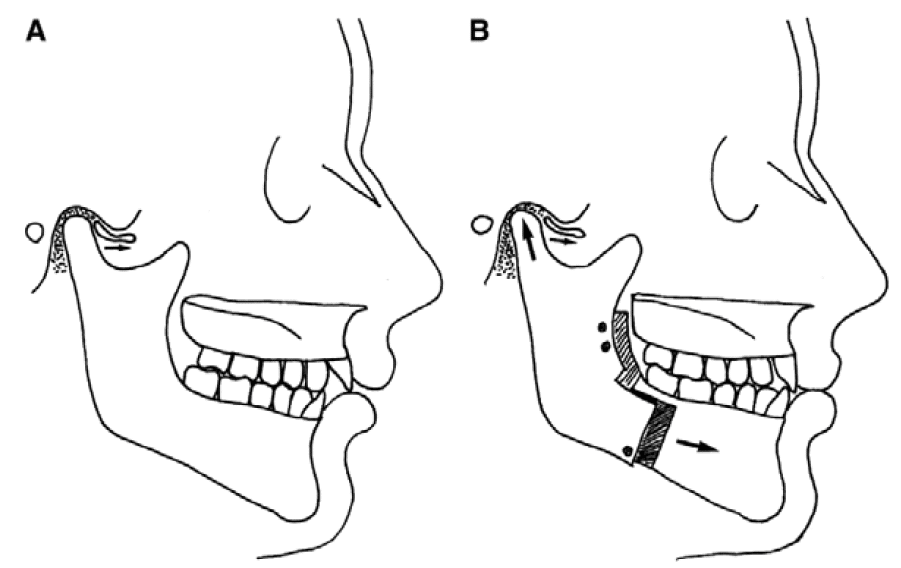
A) This illustration shows a hypoplastic mandible with a displaced TMJ articular disc.
B) The mandible is advanced without TMJ surgery. The disc will remain anteriorly displaced because the condyle will seek the most superoposterior position in the fossa when the mandible is advanced. This can initiate or worsen TMJ pain and dysfunction, headaches, condylar resorption, etc.
The TMJ surgery is done first since most TMJ procedures affect the position of the mandible (i.e., disc repositioning, high or low condylectomy). Mandibular sagittal split osteotomies with rigid fixation are done next so the mandible can be placed in the predetermined position regardless of the amount of displacement caused by the TMJ surgery.
Many TMJ patients require counter-clockwise rotation of the maxillomandibular complex to get the best functional and esthetic outcomes. In this situation it is easier to do the mandibular osteotomies before the maxillary osteotomies. If the surgeon prefers to do the TMJ surgery at a separate operation from the orthognathic surgery, then the TMJ surgery should be done first.
TMJ arthroscopy should not be used in TMJ cases requiring orthognathic surgery, as it does not provide the ability to reposition and stabilize the disc in the proper position to withstand the loading of the TMJ created from the orthognathic surgery. Arthroscopy does not “fix” the TMJ’s, so patients are highly susceptible to initiating post surgical condylar resorption and increased pain, particularly if the mandible is advanced, with requirement to repeat the orthognathic surgery as well as reconstruct the TMJs.
In addition, arthroscopy can render a reducing disc into a non-reducing disc that will then accelerate the degeneration and deformation of the articular disc, resulting in the requirement of a total joint prosthesis to eliminate the TMJ pathology and associated problems.
Wolford’s modification of the mandibular ramus sagittal split osteotomy provides an easy method to position the condyle in the fossa following TMJ surgery (Figure 24). The medial cut is made just above the lingula and the cut down the ascending ramus is made adjacent to the buccal cortex and stops distal to the second molar.
A horizontal bone cut is made perpendicular to the buccal cortex, 8 mm below the gingivocervical margin of the teeth from just distal to the 2nd molar forward 8 mm further than the amount of mandibular advancement required. This will provide a bony interface between the proximal and distal segments to control the position of the proximal segment, seat the condyle in the fossa, and accommodate a bone plate and screws.
An inferior border osteotomy is performed with a special inferior border saw and proximal and distal segments separated. The mandible is repositioned with an intermediate splint and maxillomandibular fixation applied.
The proximal segment is positioned beneath the bony ledge of the distal segment, gently pushed posteriorly at its anterior edge, and gentle finger pressure is applied externally at the angle of the mandible seating the condyle into the fossa. Rigid fixation is applied using the specially designed sagittal split bone plate (Z-plate) with 4 monocortical screws and 1 to 2 screws in the anterosuperior ramus.
The maxillary osteotomies are then performed, intranasal procedures such as septoplasty and turbinectomies completed if indicated, and rigid fixation with bone grafting to stabilize the maxilla.
Additional ancillary procedures such as genioplasty, rhinoplasty, etc. are then completed (Figure 24).
Surgical Sequencing for Orthognathic Surgery and TMJ Total Joint Prostheses Reconstruction
- Condylectomy
- Coronoidotomy or coronoidectomy
- Mobilize mandible
- Maxillomandibular fixation with intermediate surgical splint
- Placement of total joint prostheses
- Bilateral TMJ fat grafts harvested from the abdomen or buttock
- Maxillary osteotomies and mobilization
- Turbinectomies, septoplasty, etc.,
- Maxillary segmentation and application of the palatal splint if indicated
- Maxillary rigid fixation and bone grafting
- Adjunctive procedures such as genioplasty, rhinoplasty, UPPP, facial augmentation, etc.
A potential risk to patients receiving a custom-fitted or stock TMJ total joint prosthesis is infection. The occurrence rate is less than 2 % with greater risk for patients on immunosuppressant medications such rheumatoid patients or others with connective tissue/autoimmune diseases. Bacterial or viral contamination of the prosthesis can occur during surgery or develop at a later time from bacterial seeding through a hematogenic route or localized bacterial sources.
As a result, strict adherence to sterile technique for the procedures performed can prevent or reduce the chance of infection associated with the implantation of total joint prosthesis, and concomitant orthognathic surgery.
After surgical prepping including the face, neck, mouth, ears, and ear canals, the face and neck are draped, and the mouth and nose are isolated by application of a Tegaderm film dressing (Figure 25). The TMJs are approached through an endaural or pre-auricular, and submandibular incisions. A condylectomy, joint debridement, and preparation of ramus are performed followed by mobilization of mandible in a downward and forward direction.
Draping with sterile towels isolates the oral cavity. The Tegaderm is cut through and the oral cavity is entered, intermediate splint placed, and intermaxillary fixation applied. The surgeons change gloves and gown and the mouth is sealed off once again with a Tegaderm film dressing.
The total joint prostheses are inserted and fixed in position, fat grafts harvested from the abdomen or buttock are packed around the articulating area of the prostheses (Figure 26) and the incisions closed. The oral cavity is then entered, intermaxillary fixation released, and intermediate splint removed. Maxillary osteotomies are performed with rigid fixation and bone grafting as indicated followed by any other adjunctive procedures.
Special care must be taken, when performing a concomitant genioplasty procedure, with a conservative posterior dissection along the symphysis/body region to prevent communication with the total joint prosthesis implantation site. Appropriate IV antibiotics are used while in the hospital and then PO antibiotics for an additional 10 days. This patient management scheme should minimize the risk of infection.
TMJ and Facial Asymmetry:
Facial asymmetries are commonly caused by TMJ pathology and can create a progressive worsening of the facial deformity and malocclusion.[i] For example, a unilateral condylar pathological over-development of the condyle can cause facial asymmetry and affect the contralateral “normal” TMJ by creating articular disc dislocation and arthritis from the increased functional loading on that joint related to the over-development of the ipsilateral side.
Unilateral condylar under-development or resorption can cause the mandible and face to be smaller on one side and the jaws to shift toward the involved side. Performing orthognathic surgery only in facial asymmetry cases and ignoring the TMJs during treatment or failure to render proper TMJ management can result in the dentofacial asymmetry and malocclusion redeveloping with worsening TMJ associated symptoms including jaw dysfunction and pain.
Number and Type of Previous Surgeries:
Patients with TMJ articular disc dislocation, 0 to 1 previous TMJ surgeries, and no polyarticular conditions, may benefit by articular disc repositioning and ligament repair with Mitek anchors (Mitek Products Inc., Westwood, MA) to achieve a stable treatment outcome (Figure 24). Success rate is best when discs are repositioned within 4 years of initial disc displacement.
Patient with 2 or more previous TMJ surgeries will have a higher failure rate with disc repositioning or other autogenous tissue reconstruction. In these cases, a custom-fitted TMJ total joint prosthesis, (TMJ Concepts Inc. system) will have a much higher rate of success. Patients with connective tissue and autoimmune disease involvement of the TMJ will benefit from custom-fitted total joint prosthesis reconstruction since the disease processes will likely attack any autogenous tissues placed into the joint area, but will not affect TMJ total joint prostheses.
Other end-stage TMJ conditions such as severe reactive arthritis or osteoarthritis, ankylosis, severe damage from trauma, failed TMJ alloplastic implants, polyarticular conditions, etc. will get the most predictable results with custom-fitted total joint prostheses and fat grafts packed around the articulating components of the prostheses.
Repeat orthognathic surgery is technically more difficult, but usually a good result can be achieved.
Age for Surgical Intervention:
Predictability of results and limiting correction of the jaw and TMJ-related deformities to 1 major operation can best be achieved by waiting until growth is nearly complete. Although there are individual variations, girls usually have most of their facial growth (98%) complete by the age of 15 years and boys by the age of 17 to 18 years. Performing surgery at earlier ages may result in the need for additional surgery at a later time to correct a resultant deformity and malocclusion that may develop during the completion of growth.
There are definite indications for early surgery, such as progressive TMJ deterioration, ankylosis, growth center transplants (ie, rib or sternoclavicular grafts), masticatory dysfunction, tumor removal, pain, and sleep apnea. We have previously published studies on maxillary and mandibular surgery and their effects on growth with guidelines for age when considering surgical intervention.
Non-Surgical and Closed TMJ Treatment Considerations:
Nonsurgical TMJ treatments (e.g., splints, physical therapy, chiropractic treatment, orthodontics, biofeedback, acupuncture, and medications) may help the TMJ symptoms but do not stabilize and eliminate TMJ disorders (eg, disc dislocation, arthritis, condylar resorption, or condylar hyperplasia) to withstand the increased TMJ loading that usually accompanies orthognathic surgery.
Arthrocentesis and arthroscopy are contraindicated in patients with TMJ disorders requiring orthognathic surgery because these techniques do not reposition and stabilize the articular disc in a normal position, but may convert a reducing disc into a nonreducing disc that will yield a more rapid deformation and degeneration process of the disc, subsequently rendering it nonsalvageable.


