Concomitant Temporomandibular Joint (TMJ) &
Orthognathic (Corrective Jaw) Surgery
Diagnosis And Treatment Planning for TMJ Surgery
Dr. Larry M. Wolford, DMD, provides diagnosis & treatment planning for TMJ surgery prospect patients.
Temporomandibular joint (TMJ) disorders/pathology and jaw deformities commonly co-exist; therefore require an accurate diagnosis and concomitant TMJ and orthognathic (corrective jaw) surgery.
The temporomandibular joints (TMJs), jaw joints, are the foundation for jaw position, facial growth and development, function, dental occlusion, facial balance, and comfort.
Suppose the TMJs are not stable and healthy (non-pathological). In that case, patients requiring orthognathic (corrective jaw) surgery may have unsatisfactory outcomes relative to function, esthetics, dental occlusal and skeletal stability, and pain.
A review of 1369 consecutive TMJ patients referred to Dr. Larry Wolford’s practice revealed an age range of 8 to 76 years at initial evaluation, with 78% female and 22% male patients. Interestingly, 69% of the patients reported the onset of their TMJ problems during their teenage years. Therefore, TMJ pathology predominantly develops in teenage females, although it may not manifest itself until much later.
TMJ disorders/pathology and dentofacial deformities commonly co-exist. The TMJ pathology may be the causative factor of the jaw deformity, develop as a result of the jaw deformity, or the 2 entities develop independent of each other. The most common TMJ pathologies that can adversely affect jaw position, dental occlusion, as well as corrective jaw surgical outcomes include:
- TMJ Articular Disc Dislocation: Dislocation of the TMJ disc, which is positioned between the two bones that form the jaw joint.
- Adolescent Internal Condylar Resorption (AICR) of the TMJ: “Cheerleaders Syndrome” a specific condition that affects the jaw joints (temporomandibular joints or TMJs) and most commonly occurs in teenage girls.
- Reactive Arthritis of the TMJ: Frequently seen in children with chronic arthritis.
- Mandibular Condylar Hyperplasia: Slowly progressive unilateral enlargement of the head and neck of the jaw condyle causes crossbite malocclusion, facial asymmetry, and shifting of the midpoint of the chin toward the unaffected side.
- Temporomandibular Joint (TMJ) Ankylosis: The fusing together of the bones forming the joint most frequently caused by poor healing following severe trauma or infection. It can also occur congenitally, or secondary to severe rheumatoid arthritis or to tumors in the area of the TMJ.
- Congenital Deformation or Absence of the Temporomandibular Joint (TMJ): Absence of a jaw joint results in a progressively underdeveloped lower jaw that usually requires a jaw joint (TMJ) implant.
- Connective tissue and autoimmune diseases of the TMJ
- Other end-stage TMJ pathologies.1
Patients with these conditions may benefit from corrective surgical intervention including temporomandibular joint (TMJ) and orthognathic (corrective jaw) surgery. Many clinicians may have difficulty identifying the presence of a TMJ condition, diagnosing the specific TMJ pathology, and selecting the proper treatment for that condition. This website should improve the clinician’s diagnostic and treatment planning skills and give patients better understanding of their disorders and how to deal with them.
Asymptomatic TMJ pathology/disorders
Although most TMJ patients have associated symptoms, approximately 25% of patients with TMJ pathology/disorders will be asymptomatic. These patients are diagnostically challenging when undergoing orthognathic surgery because the TMJ pathology may not be recognized or treated appropriately, resulting in a poor treatment outcome with potential redevelopment of the skeletal and occlusal deformity by condylar resorption or overdevelopment as well as initiation of worsening pain, headaches, jaw and TMJ dysfunction as well as other TMJ symptoms.
Jaw surgery in the presence of displaced TMJ articular discs
The literature has clearly demonstrated the adverse affects of performing only orthognathic surgery in the presence of displaced TMJ articular discs. (2) Our research studies (3,4) show that in presence of TMJ displaced discs that are not corrected, but the maxilla and mandible are advanced, an average anteroposterior (AP) mandibular relapse of 30% can be expected as well as an 84% chance of developing or worsening of TMJ pain, facial pain, and headaches. Accurate diagnosis and proper surgical intervention for the specific TMJ pathologies that may be present in orthognathic surgery patients will provide highly predictable and stable results.
- History
- Clinical Examination
- Cephalometric Analysis
- Nasal Airway Obstruction
- Oral Airway Obstruction
- Oropharyngeal Airway Obstruction
SURGICAL TREATMENT OF OBSTRUCTIVE SLEEP APNEA
Surgical Management of Nasal Airway Obstruction
- Nostrils and Columella
- Luminal (Nasal) Valve
- Hypertrophied Turbinates
- Uvulopalatopharyngoplasty (UPPP)
- Macroglossia
- Adjunctive Procedures
- Lingual Tori and Palatal Tori
- Tonsils and Adenoid Tissue
DIAGNOSTIC IMAGING OF THE TEMPOROMANDIBULAR JOINT (TMJ)
- Connective Tissue / Autoimmune Diseases:
- Silent TMJ with Disc Displacement:
- Adolescent Internal Condylar Resorption (AICR)
- Osteochondroma (Condylar Hyperplasia [CH] Type 2)
- Reactive Arthritis
Perforations of the TMJ
- Synovial Cysts within the TMJ
COMPREHENSIVE DIAGNOSTIC LIST AND TREATMENT PLAN
Intraoperative Surgical Sequencing:
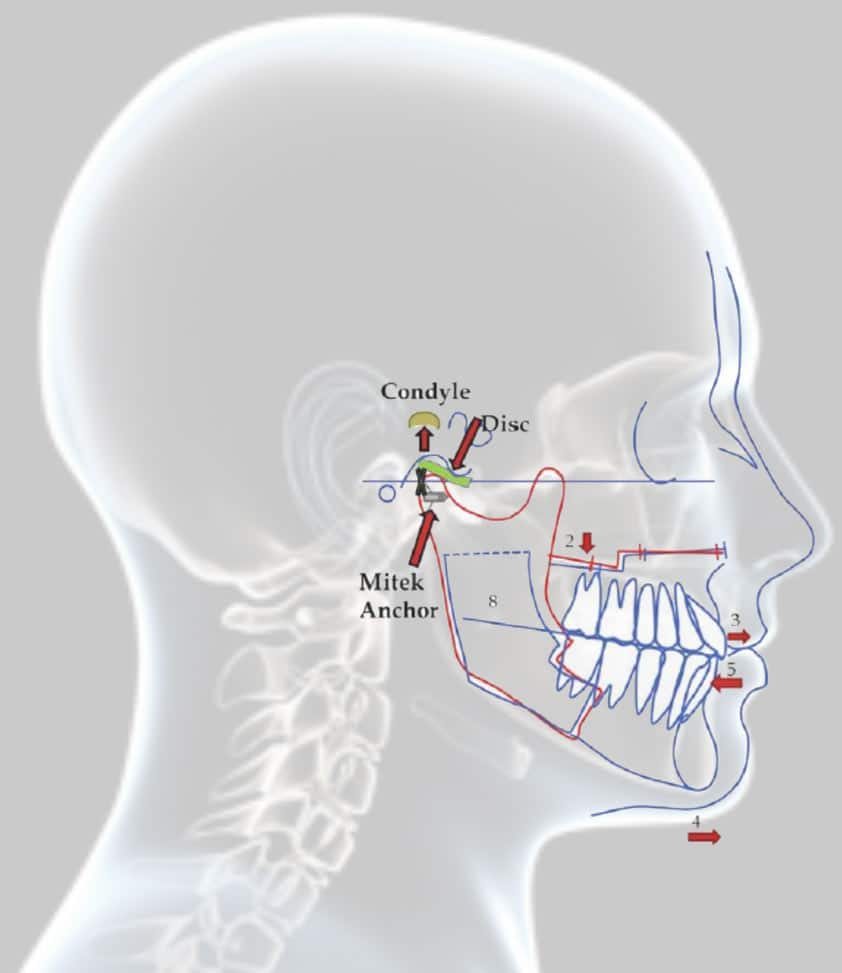
Surgical Sequencing in Orthognathic Surgery in Combination with Disc Repositioning:
Surgical Sequencing for Orthognathic Surgery and TMJ Total Joint Prostheses Reconstruction:
- Condylectomy
- Coronoidotomy or coronoidectomy
- Mobilize mandible
- Maxillomandibular fixation with intermediate surgical splint
- Placement of total joint prostheses
- Bilateral TMJ fat grafts harvested from the abdomen or buttock
- Maxillary osteotomies and mobilization
- Turbinectomies, septoplasty, etc.,
- Maxillary segmentation and application of the palatal splint if indicated
- Maxillary rigid fixation and bone grafting
- Adjunctive procedures such as genioplasty, rhinoplasty, UPPP, facial augmentation, etc.
Number and Type of Previous Surgeries:
Age for Surgical Intervention:
Non-Surgical and Closed TMJ Treatment Considerations
CONDYLAR OVER-DEVELOPMENT CONDITIONS
- Condylar Hyperplasia Type 1 Case 1
- Condylar Hyperplasia Type 2; Osteochondroma Or Osteoma Case 2
CONDYLAR UNDERDEVELOPMENT- RESORPTION CONDITIONS
- Articular Disc Dislocation
- Adolescent Internal Condylar Resorption (AICR) Cases 3 And 4
- Reactive Arthritis Cases 5 And 6
- Trauma
- TMJ Ankylosis Case 7
- Congenital Deformed/Absent TMJ (Hemifacial Microsomia) Case 8
- Connective Tissue And Autoimmune Diseases (CT/AI) Cases 9 And 10
- Other End-Stage TMJ Pathology
Dr. Wolford has been a pioneer in the treatment of many of these syndromes and has developed procedures to provide high quality outcomes for these patients. At your consultation, Dr. Wolford will develop a diagnosis and comprehensive treatment plan to correct your problems. Please contact Dr. Larry Wolford’s office using our online contact form or call 214-828-9115 if you would like to schedule an appointment.