Adolescent Internal Condylar Resorption (ACIR) Cases 3 and 4
Adolescent Internal Condylar Resorption – AICR is one of the most common TMJ conditions seen in teenage females (8:1, female: male).
This hormonally mediated condition is initiated as the adolescent enters the pubertal growth phase (age of onset between 11 to 15 years).
The TMJ articular discs become anteriorly displaced and the condylar heads resorb with slow but progressive retrusion of the mandible creating a Class II occlusal relation and commonly an anterior open bite.
25% of patients with AICR are asymptomatic relative to pain and joint noises but still have the displaced discs and condylar resorption. All patients have high occlusal plane angulation with a retruded mandibular facial morphology MRI will show anteriorly displaced discs, small condyles, and amorphous tissue (hyperplasia of synovial cells and non-inflammatory) surrounding the condyles.
When the discs are still salvageable, our treatment protocol has proven to eliminate this TMJ pathology and allow optimal correction of the associated dentofacial deformity at the same operation. The protocol includes:
- Remove the tissue surrounding the condyle
- Reposition and stabilize the disc to the condyle with a Mitek anchor and artificial ligaments
- Perform the indicated double jaw orthognathic surgery with counter-clockwise rotation of the maxilla-mandibular complex, and any other adjunctive procedures that are indicated.(Case 3)
Because of the high occlusal plane angle and retruded mandible and maxilla, with posterior vertical maxillary hypoplasia, counter-clockwise rotation of the maxillomandibular complex can yield the best functional and esthetic outcomes. Because this high angle facial morphology is commonly associated with decreased oropharyngeal airway space and sleep apnea, the counter-clockwise rotation of the maxillomandibular complex will also maximize the A-P dimension of the oropharyngeal airway, eliminating sleep apnea symptoms.
Our studies and others have shown that performing only orthognathic surgery on AICR patients will result in predictable continued condylar resorption with subsequent skeletal relapse, redevelopment of a Class II anterior open bite and increased pain. Our treatment protocol has proven to eliminate this TMJ pathology, produce stable Class I occlusal outcomes with elimination of pain, improved jaw function, and good facial balance. In advanced AICR pathology with non-salvageable discs, total joint prostheses with fat grafts may be indicated to reconstruct the TMJs and advance the maxillomandibular complex in a counter-clockwise direction.

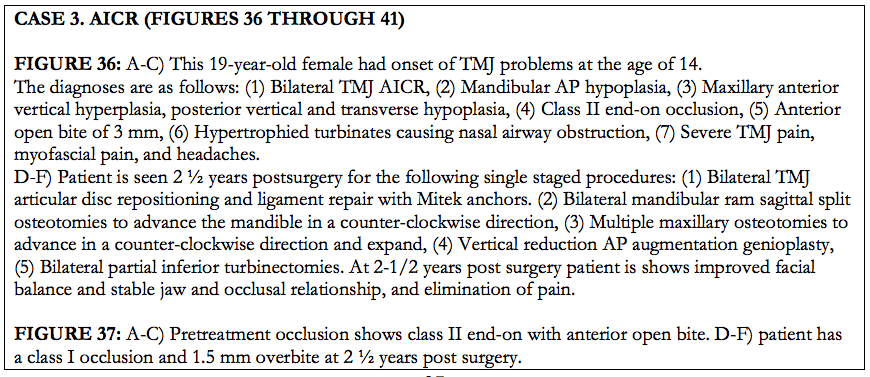
Figure 36, Case 3: A-C) Presurgery clinical images, D-F) Postsurgery clinical images, at 2 ½ years.
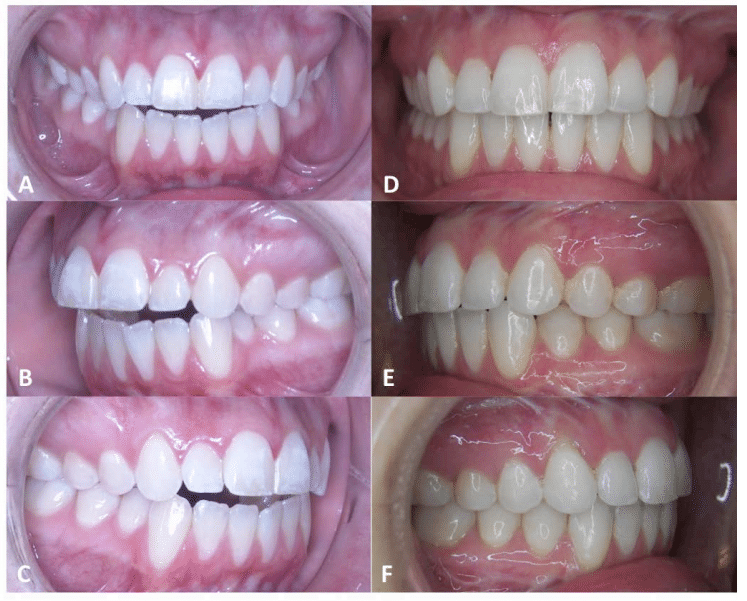
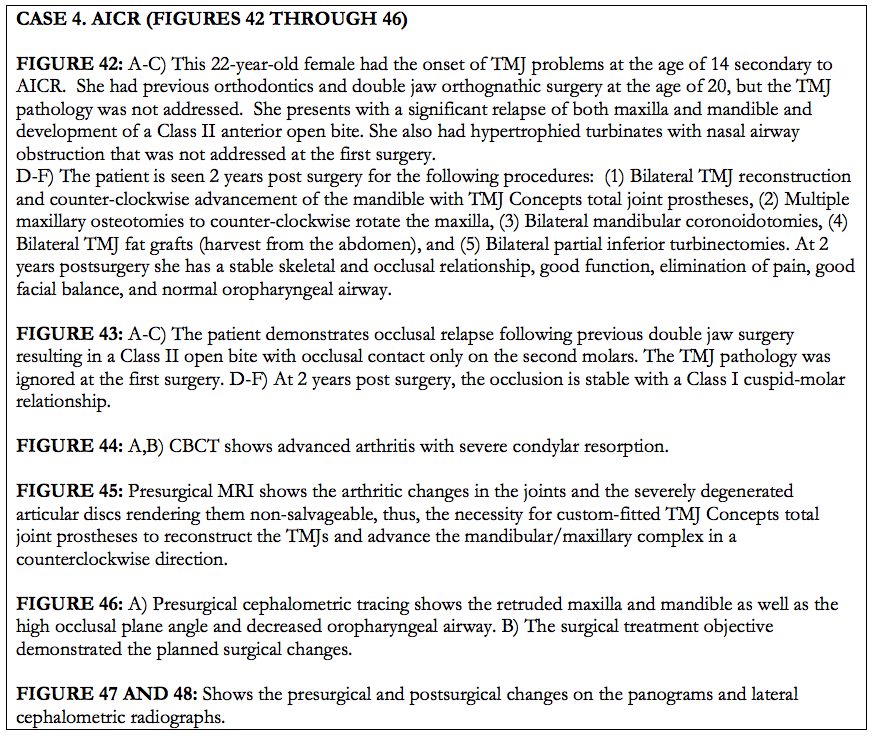
Figure 37, Case 3: A-C) Presurgery intraoral pictures, D-F) Postsurgery intraoral picture at 2 ½ years.
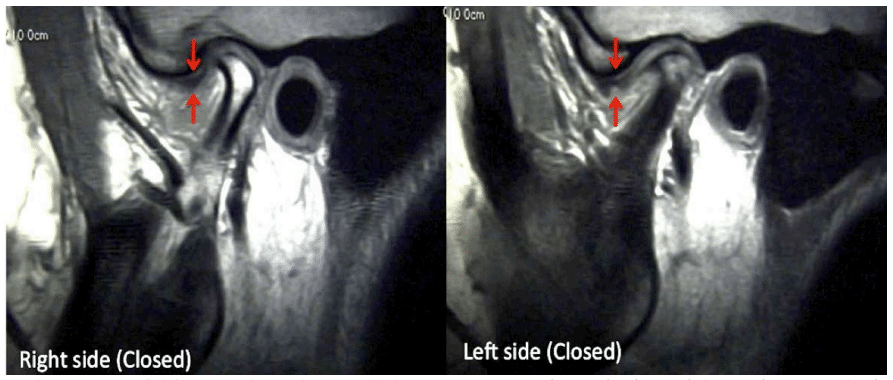
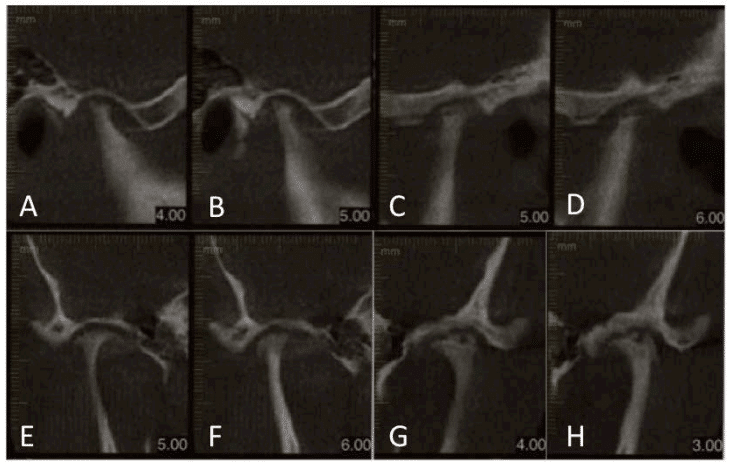
Figure 38, Case 3: Bilateral sagittal T1 MRI images of resorbed condyles and anteriorly displaced discs.
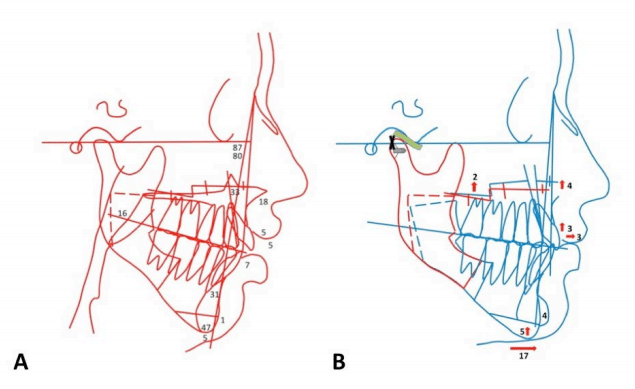
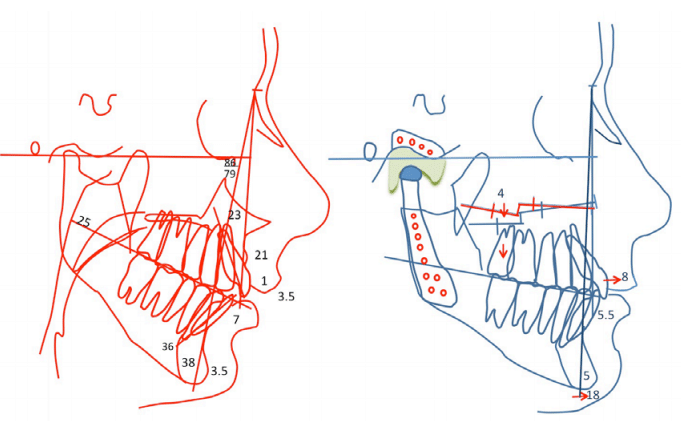
Figure 39, Case 3: A) Presurgery cephalometric tracing, B) Surgical treatment objective tracing.
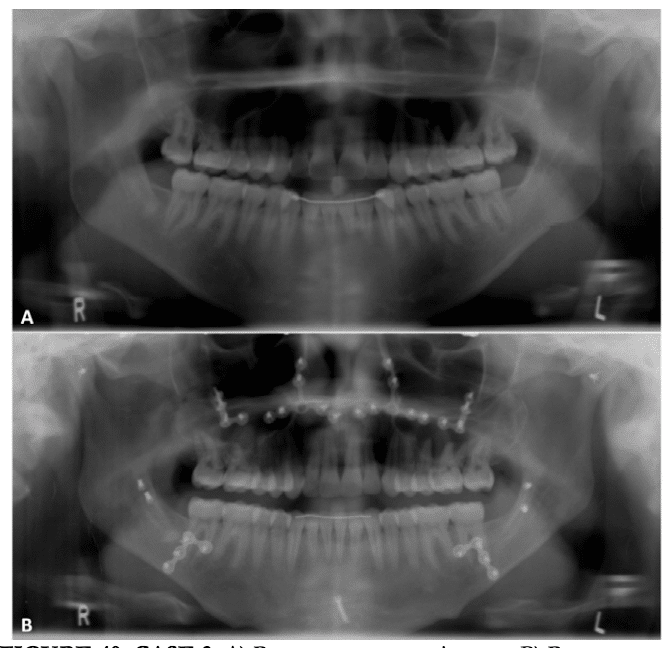
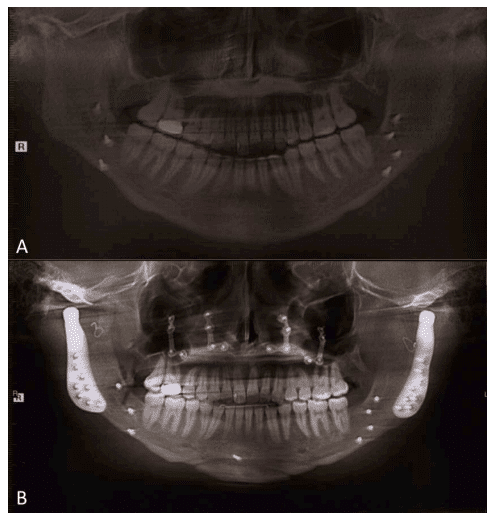
Figure 40, Case3: A) Presurgery panoramic x-ray, B) Postsurgery panoramic x-ray at 2 ½ years.
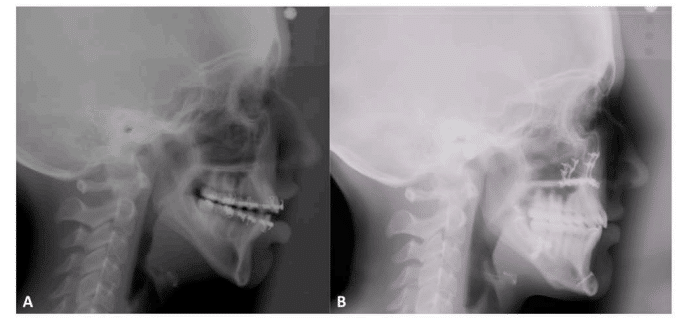
Figure 41, Case 3: A) Presurgery cehpalometric x-ray, B) Postsurgery cephalometric x-ray at 2 ½ years.
Case 4. AICR (Figures 42 Through 46)
Figure 42:
A-C) This 22-year-old female had the onset of TMJ problems at the age of 14 secondary to AICR. She had previous orthodontics and double jaw orthognathic surgery at the age of 20, but the TMJ pathology was not addressed. She presents with a significant relapse of both maxilla and mandible and development of a Class II anterior open bite. She also had hypertrophied turbinates with nasal airway obstruction that was not addressed at the first surgery.
D-F) The patient is seen 2 years post surgery for the following procedures: (1) Bilateral TMJ reconstruction and counter-clockwise advancement of the mandible with TMJ Concepts total joint prostheses, (2) Multiple maxillary osteotomies to counter-clockwise rotate the maxilla, (3) Bilateral mandibular coronoidotomies, (4) Bilateral TMJ fat grafts (harvest from the abdomen), and (5) Bilateral partial inferior turbinectomies. At 2 years postsurgery she has a stable skeletal and occlusal relationship, good function, elimination of pain, good facial balance, and normal oropharyngeal airway.
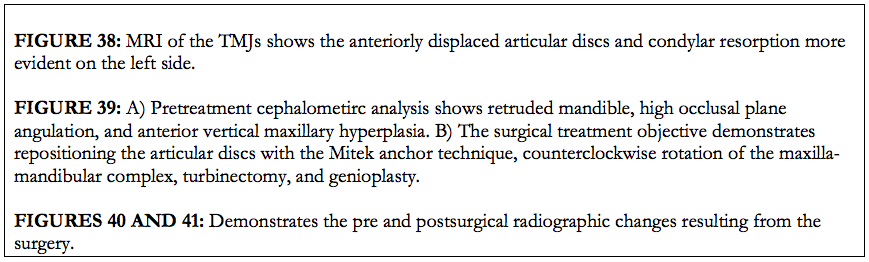
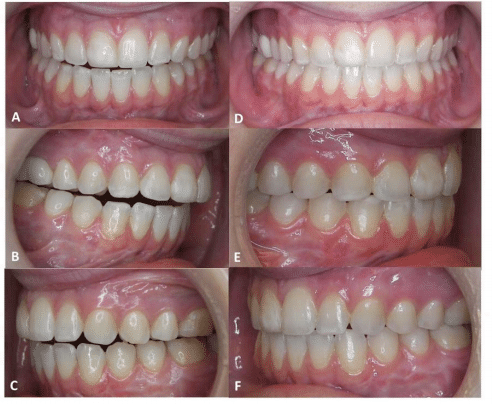
Figure 43:
A-C) The patient demonstrates occlusal relapse following previous double jaw surgery resulting in a Class II open bite with occlusal contact only on the second molars. The TMJ pathology was ignored at the first surgery.
D-F) At 2 years post surgery, the occlusion is stable with a Class I cuspid-molar relationship.
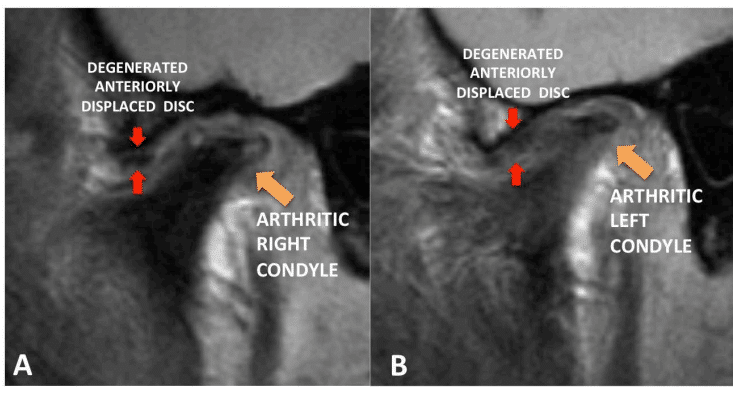
Figure 44: A,B) CBCT shows advanced arthritis with severe condylar resorption.
Figure 45: Presurgical MRI shows the arthritic changes in the joints and the severely degenerated articular discs rendering them non-salvageable, thus, the necessity for custom-fitted TMJ Concepts total joint prostheses to reconstruct the TMJs and advance the mandibular/maxillary complex in a counterclockwise direction.
Figure 46: A) Presurgical cephalometric tracing shows the retruded maxilla and mandible as well as the high occlusal plane angle and decreased oropharyngeal airway. B) The surgical treatment objective demonstrated the planned surgical changes.
Figure 47 and 48: Shows the presurgical and postsurgical changes on the panograms and lateral cephalometric radiographs.
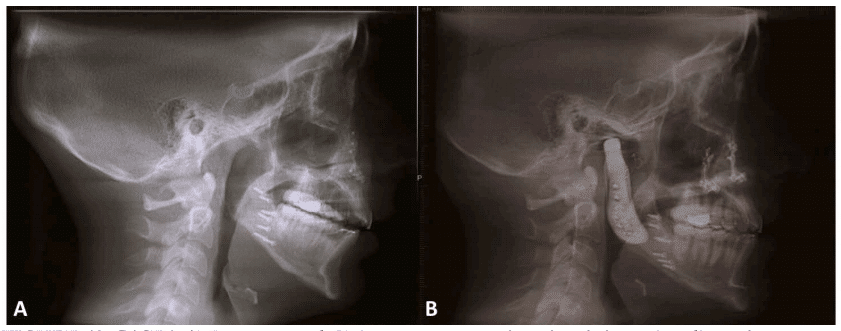
Figure48, Case 4: A) Presurgery and, B) 2 year post surgery lateral cephalometric radiograph.