Connective Tissue and Autoimmune Diseases (CT/AI) (Cases 9 and 10)
CT/AI – Connective Tissue and Autoimmune diseases that can affect the TMJs include:
- Rheumatoid arthritis,
- juvenile rheumatoid arthritis,
- juvenile idiopathic condylar resorption,
- psoriatic arthritis,
- ankylosing spondylitis,
- Sjogren’s syndrome,
- systemic lupus erythema,
- scleroderma,
- mixed connective tissue disease, etc.
Multiple systems are usually involved. Peripheral joints are usually symmetrically inflamed resulting in progressive destruction of articular structures. Joints are usually affected bilaterally.
Facial deformity can occur with involvement of the TMJs. Clinical and radiographic features when the TMJs are involved with condylar resorption includes:
- Retruded mandible;
- Posterior maxillary vertical hypoplasia,
- Progressive worsening facial and occlusal deformity;
- High occlusal plane angle;
- Class II occlusion and anterior open bite; and
- TMJ symptoms such as noises, pain, jaw dysfunction, etc.
MRI features include: Loss of condylar vertical dimension, significant medio-lateral condylar narrowing but the condyles may mushroom and become broad in the A-P direction; articular disc may be in position but surrounded by a pannus (reactive tissue) that eventually destroys the disc but also causes condylar and articular eminence resorption.
In more severe cases, the condylar stump may function beneath the remaining articular eminence or anterior to it.
The most predictable treatment for the TMJ affected by CT/AI diseases includes:
- Bilateral reconstruction of the TMJs (and if indicated, advancement of the mandible) with custom-fitted total joint prostheses (TMJ Concepts system;
- Coronoidotomies or coronoidectomies if the ramus is significantly advanced or vertically lengthened with the prostheses;
- Autogenous fat graft harvested form the abdomen or buttock, packed around the prosthesis in the articulation area; and
- Maxillary osteotomies and any additional adjunctive procedures indicated (i.e. genioplasty, rhinoplasty, turbinectomies, septoplasty, etc.
Other techniques that have been advocated for TMJ reconstruction include using autogenous tissues such as temporal fascia and muscle flaps, dermal grafts, rib grafts, sternoclavicular grafts, vertical sliding ramus osteotomy, etc.
However, the CT/AI disease process that created the original TMJ pathology can attack the autogenous tissues used in the TMJ reconstruction causing failure of the grafts. The total joint prosthesis with a fat graft packed around it is a superior technique relative to elimination of the CT/AI disease process in the TMJ, improved function and esthetics, and eliminate or decrease pain.
Our studies have demonstrated that performing reconstruction with counter-clockwise rotation of maxilla-mandibular complex is a very stable procedure with good jaw function, decrease in pain, and significant increased dimension of the oropharyngeal airway, eliminating sleep apnea issues.
When treating young growing patients (10 years or older), the total joint prosthesis may still be the best option to eliminate the CT/AI disease process. However, since there would be no growth potential on the involved side(s) of the mandible, orthognathic surgery may be necessary, but can be delayed until the patient has most of the facial growth complete (age 15 for females and age 17 for males).
Then double jaw surgery can be performed, including the sagittal split on the side of the prosthesis to reposition the jaws into the best alignment, or repositioning of the mandibular component of the prosthesis, or manufacturing a new longer mandibular component to advance the mandible.
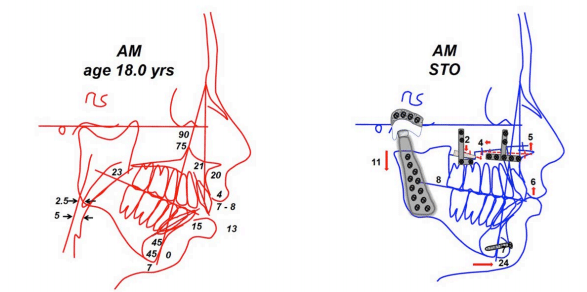
FIGURE 61:
A-C) This 18-year-old female presented with juvenile rheumatoid arthritis (JRA), bilateral TMJ involvement with significant and progressive condylar resorption, retruded maxilla and mandible, class II skeletal and occlusal dentofacial deformity, anterior open bite, decreased oropharyngeal airway with sleep apnea symptoms, and TMJ pain and headaches.
D-F) The patient is seen 2 years post surgery for the following procedures:
- Bilateral TMJ reconstruction and mandibular counterclockwise advancement with custom-fitted TMJ total joint prostheses (TMJ Concepts system);
- Bilateral TMJ fat grafts (harvest from abdomen) packed around the functional component of the prostheses;
- Bilateral coronoidectomies;
- Multiple maxillary osteotomies to down graft the posterior aspect and upright the incisors; and
- Chin augmentation with an alloplastic implant.
FIGURE 62
(A-C): The pre-surgical occlusion demonstrated an anterior open bite and Class II end-on cuspid relationship.
FIGURE 63:
A) Presurgical cephalometirc analysis shows the retruded maxilla and mandible, high occlusal plane angulation, and decreased oropharyngeal airway.
B) Surgical treatment objective illustrates the planned procedures to advance the maxilla-mandibular complex in a counterclockwise direction, advancing pogonion 24 mm, including an alloplastic chin implant.
FIGURE 62 (D-F): The occlusion remained stable at two year postsurgery.

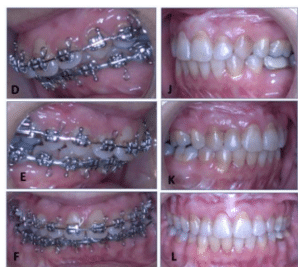
Figure 61, Case 9: A-C) Presurgery clinical images of 18 year old female with JRA, D-F) Postsurgery clinical images of the patient at 2 years follow-up.
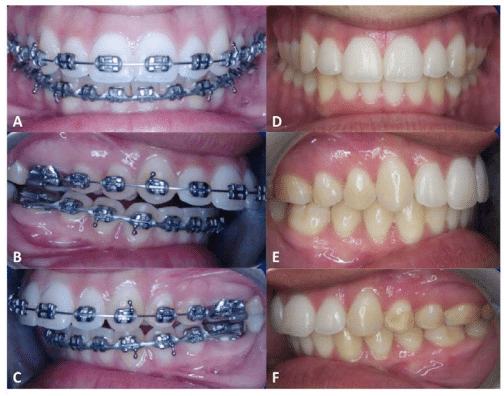
Figure 62, Case 9 – CT/AI: A-C) Presurgery and D-F) Postsurgery photos at 2 years follow-up.
A) Presurgery cephalometric analysis, demonstrating the significant deformity including Retruded maxilla and mandible, Class II occlusion, high occlusal plane angle, and decreased oropharyngeal airway.
B) Surgical treatment object tracing showing the planned surgical changes.
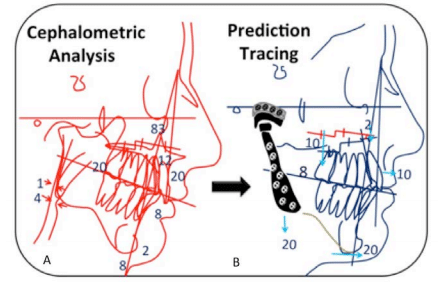
Case 10 – CT/AI (Figures 64 Through 69)
Figure 64
(A-F): This 46-year-old female was diagnosed with juvenile rheumatoid arthritis (JRA) at age 8. Her presurgical diagnoses included:
- Bilateral TMJ JRA with severe condylar resorption;
- Mandibular and maxillary hypoplasia;
- Decreased oropharyngeal airway and sleep apnea;
- Hypertrophied turbinates causing nasal airway obstruction;
- Hyperplastic soft palate and uvula; and
- Class II occlusion. Incisal opening was 29 mm and excursion movements were right 3 mm and left 1 mm. She had previous orthodontics beginning at age 4 and finishing at age18 with 4 bicuspid extractions and headgear. Previous surgery included an osseous genioplasty.
D-F) Patient is seen 4 years postsurgery following a one stage surgery that included:
- Bilateral TMJ reconstruction and mandibular advancement in a counter-clockwise direction with TMJ Concepts custom fitted total joint prostheses (pogonion advanced 20 mm);
- Multiple maxillary osteotomies for counter- clockwise rotation advancement (incisor edges advanced 10 mm);
- Bilateral TMJ fat grafts (harvested from the abdomen);
- Bilateral coronoidotomies;
- Bilateral partial inferior turbinectomies; and
- Uvulopalatopharyngeoplasty (UPPP). At 4 years post surgery she demonstrates good facial balance, Class I occlusion, no pain, elimination of sleep apnea, and an incisal opening of 32 mm with 3 mm of excursion in each direction.
Figure 65:
A-C) The patient had extensive prior orthodontics resulting in her current class II end – occlusion.
D-F) at the 4 years post surgery, her occlusion is class I and stable.
Figure 66:
A) Presurgical cephalometric analysis shows the retruded maxilla and mandible, high occlusal plane, and decreased oropharyngeal airway.
B) The surgical treatment objective projects the anticipated movement with maxillary incisors advancing 10 mm and pogonion 20 mm.

Figure 64, Case 10: A-C) Presurgical and G-I) Post surgery clinical photographs, with improved facial balance and esthetics, at 4 years follow-up.
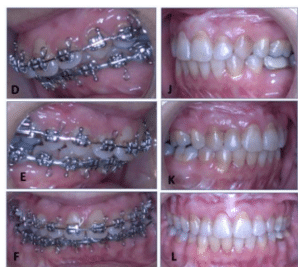
Figure 65, Case 10: D-F) Presurgery and J-L) Post surgery occlusal images at 4 years follow-up.
A) Presurgical lateral cephalometric analysis shows significant retrusion of the mandible and maxilla, high occlusal plane angulation, as well as the decreased oropharyngeal airway.
B) Th surgical treatment objective tracing shows the counterclockwise rotation of the maxillary and mandibular complex with improved facial balance with pogonion advancing 20 mm and maxillary incisors advancing 10 mm.
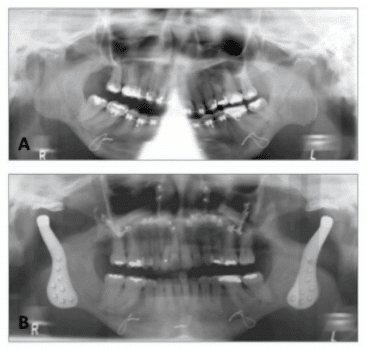
A) Presurgery panogram shows the severe TMJ arthritis, resorption of the eminence, and forward positioning of the condyles; common findings in JRA patients,
B) 4 year post surgery panogram. The space between the metal component of the fossa and condylar head of the prostheses represents the polyethylene of the fossa component.
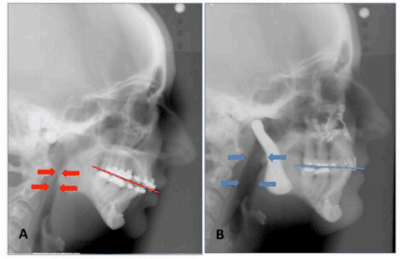
A) Lateral cephalometric radiograph shows the presurgery position of the maxilla and mandible with severe retrusion, high occlusal plane angle, and decreased oropharyngeal airway.
B) Postsurgical lateral cephalogram shows the skeletal and occlusal changes as well as the increased oropharyngeal airway. The TMJs have been reconstructed and mandible advanced with bilateral custom fitted TMJ Concepts total joint prostheses.
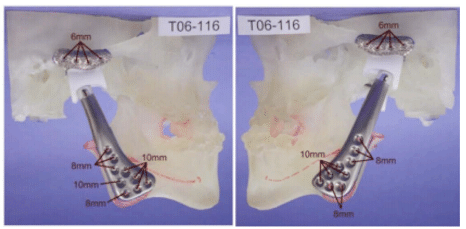
Figure 69, Case 10: The stereolithographic model was constructed from the special CT scan protocol. The mandible was counter-clockwise rotated and placed into its predetermined final position and secured to the maxilla. The TMJ Concepts patient-fitted total joint prostheses were then constructed on the 3-D model to fit the patient’s specific anatomical requirements.