Craniofacial defects are a category of congenital conditions that affect the development of the head, face, and skull. They are more common than many people realize and can range from minor aesthetic differences to complex structural challenges that impact essential functions like breathing, eating, and vision.
Among these wide-ranging conditions, one defect stands out as the most prevalent. In this article, we’ll explore what craniofacial defects are, with a detailed look at the most common condition, its causes, diagnosis, and treatment options. Whether you’re a parent seeking answers, a medical professional broadening your knowledge, or a researcher deepening your expertise, this guide is for you.
Understanding Craniofacial Defects
Craniofacial defects refer to abnormalities in the structure of the head and face that occur during fetal development. These conditions are generally congenital, meaning they are present at birth, and can range in severity from mild cosmetic irregularities to life-threatening complications.
Some craniofacial defects affect the bones of the skull, while others involve soft tissue, such as muscles and skin. Common examples include cleft lip and palate, craniosynostosis, and hemifacial microsomia. These conditions not only affect physical appearance but may also impact critical functions such as breathing, speaking, or hearing.
Craniofacial defects often require specialized care from multidisciplinary teams of healthcare providers, including surgeons, orthodontists, speech therapists, and psychologists. Early intervention is key to achieving the best possible outcomes.
How Craniofacial Development Works
To better understand craniofacial defects, it’s helpful to first grasp basic craniofacial development. During pregnancy, a baby’s face forms between the 4th and 10th weeks of gestation. This process involves the intricate fusion of tissues and bones.
Typically, the left and right sides of the face develop separately and then meet at the midline. If this process is disrupted for any reason, gaps or malformations may occur. Genes and environmental factors both play a role in regulating this complex process, meaning even slight missteps can lead to defects.
Understanding this development underpins our ability to identify, prevent, and treat craniofacial anomalies.
The Most Common Craniofacial Defect
The most common craniofacial defect is cleft lip and palate, which is estimated to affect 1 in 700 live births globally. This condition occurs when the tissue that forms the lip or roof of the mouth (palate) does not fully fuse during early pregnancy, leaving a gap.
Clefts can appear as:
- Cleft Lip – A gap in the upper lip, which can range from a small notch to a significant opening that extends into the nose.
- Cleft Palate – An opening in the roof of the mouth that may expose the nasal cavity to the oral cavity.
- Both Cleft Lip and Palate – Some children are born with both conditions simultaneously.
Cleft lip can be unilateral (on one side of the lip) or bilateral (on both sides). This defect impacts not only the aesthetics of the face but also essential functions, such as eating, speaking, and breathing.
Causes and Risk Factors for Cleft Lip and Palate
Scientists and medical professionals agree that cleft lip and palate arise from a mix of genetic and environmental factors, though no single cause can be pinpointed.
Genetic Factors
Mutations or alterations in specific genes that regulate craniofacial development can increase the likelihood of a baby being born with a cleft. If one or both parents have had a cleft, the likelihood of passing it on to their child increases.
Environmental Triggers
Environmental factors during pregnancy can also play a role. Here are notable risk factors:
- Smoking or Alcohol Use: Harmful substances during pregnancy can hinder fetal development.
- Nutritional Deficiencies: A lack of folic acid, a vital nutrient, has been associated with an increased risk of cleft lip and palate.
- Medications: Certain anti-seizure medications, acne drugs, or steroids taken during pregnancy may interfere with facial development.
- Maternal Illnesses: Conditions such as diabetes are linked to a higher risk of cleft lip and palate.
While individual risk factors may raise concern, it’s essential to remember that clefts often occur without an obvious cause and are not typically anyone’s “fault.”
Diagnosing Cleft Lip and Palate
Fortunately, prenatal and postnatal diagnostic tools make identifying cleft lip and palate relatively straightforward.
During Pregnancy
Cleft lip is often detected during a routine ultrasound scan, typically around 20 weeks of gestation. However, cleft palate is more difficult to diagnose prenatally because it is located inside the mouth and not always easily visible on ultrasound.
After Birth
A physical examination of the baby’s mouth, lips, and palate confirms the diagnosis. Further tests, such as imaging scans, may be conducted to evaluate the severity of the condition and plan treatment.
Treatment Options for Cleft Lip and Palate
Cleft lip and palate are highly treatable, especially with early intervention. Treatment plans are typically tailored to the individual’s specific needs and often begin soon after birth.
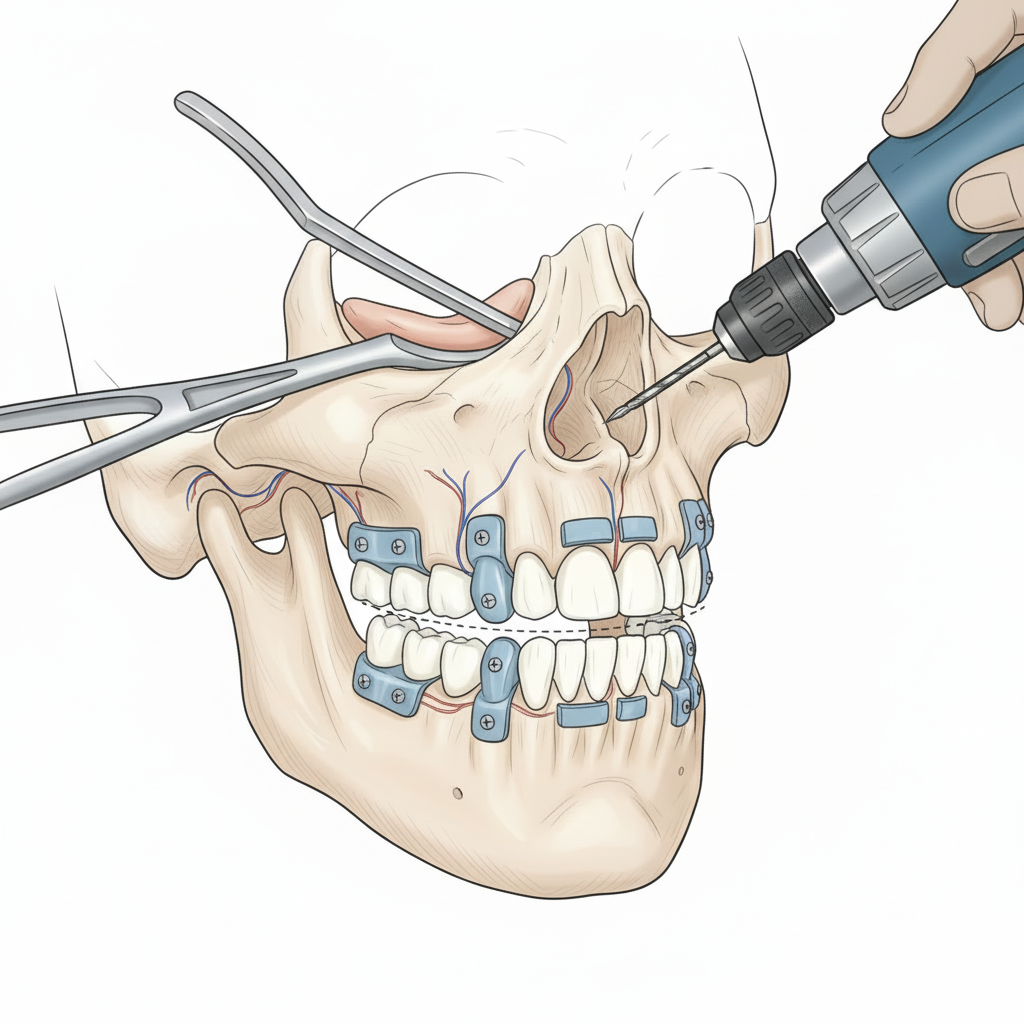
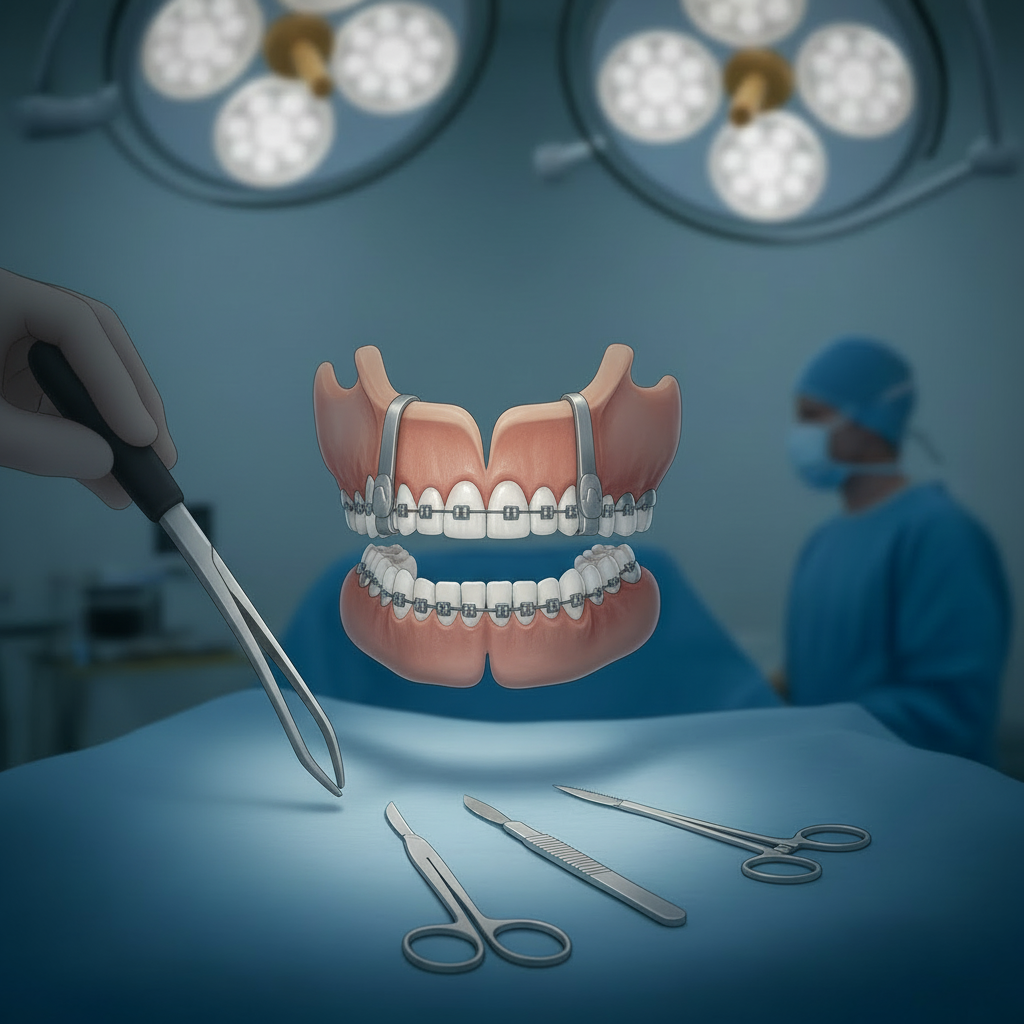
Surgical Repair
Surgery is the primary treatment for cleft lip and palate.
- Cleft Lip Repair: Generally performed when the baby is 3 to 6 months old. This surgery closes the gap in the lip and creates a more natural appearance.
- Cleft Palate Repair: Performed between 9 and 18 months of age. This surgery closes the roof of the mouth to improve feeding, speech, and other functions.
- Some individuals may require additional surgeries during adolescence to refine their appearance or improve functionality.
Additional Therapies
- Speech Therapy: Speech therapists work with children to overcome speech difficulties caused by the cleft.
- Orthodontic Care: Braces and other dental treatments may be necessary to correct teeth alignment.
- Psychological Support: Counseling can help children and their families build confidence and cope with social challenges.
Support and Resources for Families
Raising a child with cleft lip and palate can be emotionally and financially demanding, but there are many resources available to support families.
- Cleft-specific Organizations: Groups like Smile Train and Operation Smile provide free or low-cost surgeries to families in need.
- Community Groups: Online and local support groups allow parents to share experiences and advice with others facing similar challenges.
- Hospital Networks: Many medical centers have craniofacial teams that include surgeons, social workers, and support staff dedicated to guiding families through their treatment journeys.
Raising Awareness and Supporting Families
Cleft lip and palate, as the most common craniofacial defect, provide a critical starting point for increasing awareness about craniofacial conditions. Understanding the causes, risk factors, treatments, and resources ensures better outcomes for affected children, while empowering families with the knowledge and support they need.
Parents, medical professionals, and researchers have a shared responsibility to advocate for early intervention and access to care. By working together, we can make sure every child born with a craniofacial defect gets the chance to thrive.
If you want to learn more or connect with organizations that support families, take the next step today. Every small action builds toward greater awareness and better care.