Are you suffering from chronic jaw pain, headaches, or difficulty chewing? TMJ (temporomandibular joint) disorders might be the culprit behind your discomfort. In severe cases, TMJ surgery could be the solution you need to find relief and regain your quality of life.
In this comprehensive guide, we will walk you through everything you need to know about TMJ surgery. From understanding the causes and symptoms of TMJ disorders to exploring the various surgical options available, we’ll provide you with the information you need to make an informed decision about your treatment.
Our expert team of healthcare professionals will share valuable insights and dispel common misconceptions about TMJ surgery. We will also explore alternative treatments and lifestyle adjustments that may complement surgical interventions. Whether you’re a potential candidate for TMJ surgery or simply seeking to expand your knowledge on the topic, this article will serve as your go-to resource.
Don’t let TMJ disorders control your life any longer. Read on to empower yourself with the knowledge you need to take control of your oral health and well-being.
What is TMJ surgery?
TMJ (Temporomandibular Joint) surgery is a medical procedure that is performed to address severe and chronic issues related to the jaw joint. The temporomandibular joint is the hinge that connects the lower jaw (mandible) to the temporal bone of the skull, allowing for the opening and closing of the mouth. When this joint becomes dysfunctional or damaged, it can lead to a range of painful and debilitating symptoms, collectively known as TMJ disorders.
TMJ surgery is typically considered as a last resort option when non-surgical treatments have failed to provide relief or when the condition has significantly impacted a person’s quality of life. The main goal of TMJ surgery is to restore the proper function and alignment of the jaw joint, alleviate pain, and improve the individual’s ability to chew, speak, and perform other daily activities without discomfort.
There are various types of TMJ surgeries, each tailored to address specific issues related to the joint. These procedures can range from minimally invasive arthroscopic techniques to more complex open-joint surgeries. The choice of surgical approach depends on the severity of the TMJ disorder, the underlying cause, and the individual’s specific needs and preferences. It is essential to work closely with a qualified oral and maxillofacial surgeon to determine the most appropriate treatment plan for your condition.
Common causes of TMJ disorders
TMJ disorders can arise from a variety of factors, both physical and psychological. Understanding the potential causes of TMJ issues is crucial in determining the most effective course of treatment, including the potential need for surgical intervention.
One of the most common causes of TMJ disorders is trauma to the jaw, such as a blow to the face, a car accident, or a sports injury. These types of physical injuries can damage the joint, leading to inflammation, pain, and restricted movement. Additionally, conditions that involve grinding or clenching the teeth (bruxism) can also contribute to TMJ problems by placing excessive stress on the jaw joint.
Arthritis, particularly osteoarthritis or rheumatoid arthritis, can also affect the temporomandibular joint, causing joint degeneration and pain. Certain genetic factors and congenital abnormalities in the jaw structure may also predispose individuals to TMJ disorders. Furthermore, stress and anxiety can play a significant role in the development and exacerbation of TMJ issues, as these psychological factors can lead to increased muscle tension and clenching of the jaw.
In some cases, the underlying cause of a TMJ disorder may not be readily apparent, making the diagnosis and treatment more challenging. Regardless of the specific cause, it is essential to seek medical attention from a qualified healthcare provider to properly assess and address the issue.

Symptoms of TMJ disorders
TMJ disorders can manifest a wide range of symptoms, which can vary in severity and impact an individual’s daily life. Understanding the common symptoms associated with TMJ issues is crucial in recognizing the need for medical intervention, including the potential for TMJ surgery.
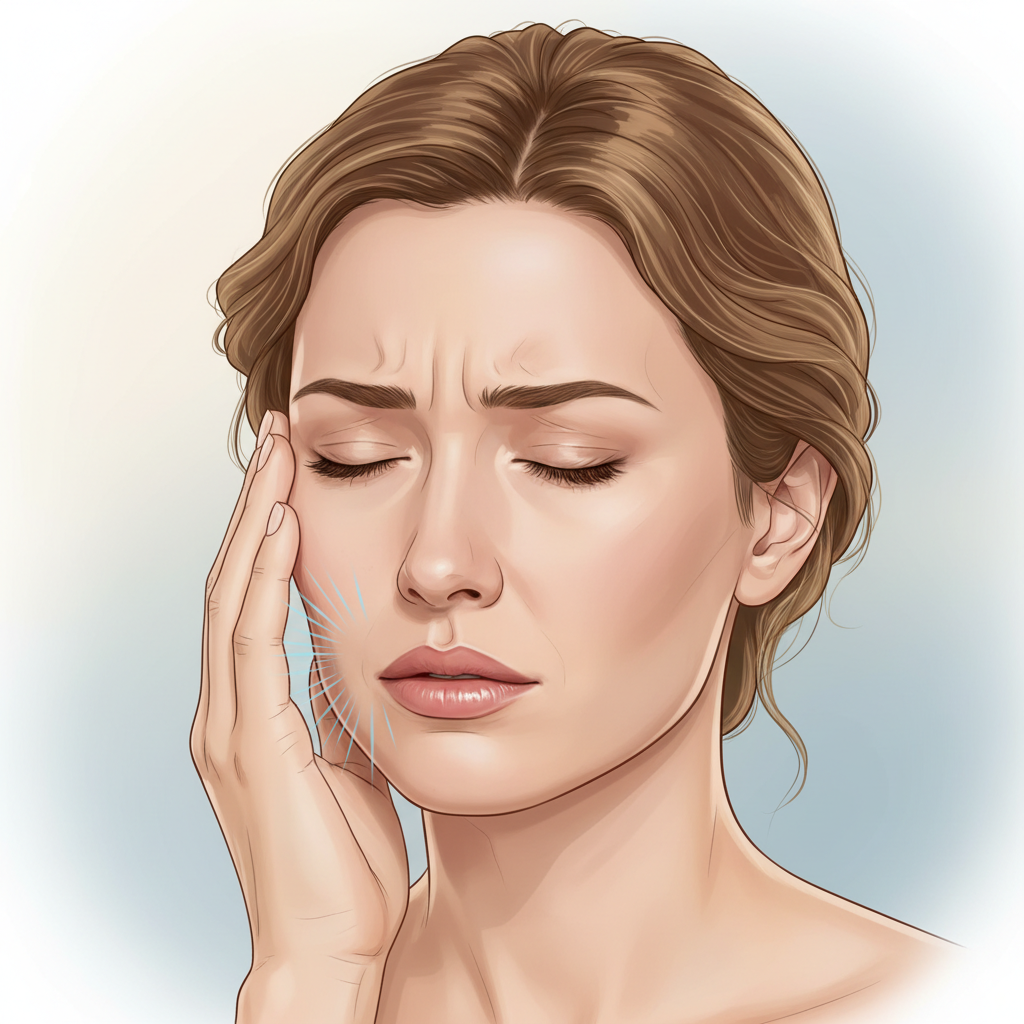
One of the most prevalent symptoms of TMJ disorders is pain in the jaw joint, facial muscles, or the area around the ear. This pain can be persistent or intermittent, and it may worsen with jaw movement, chewing, or clenching the teeth. Patients may also experience headaches, earaches, or a feeling of pressure or fullness in the ears.
Another common symptom of TMJ disorders is difficulty opening the mouth, often referred to as “limited jaw movement” or “jaw locking.” This can make it challenging to perform basic tasks such as eating, yawning, or brushing one’s teeth. In some cases, the jaw may get stuck in an open or closed position, requiring medical intervention to release it.
TMJ disorders can also cause clicking, popping, or grinding sounds when opening and closing the mouth. These noises are often accompanied by a sensation of the jaw joint catching or sticking during movement. Additionally, some individuals with TMJ issues may experience dizziness, neck and shoulder pain, or even changes in their bite alignment or the way their teeth fit together.
It is important to note that the severity and combination of symptoms can vary greatly among individuals with TMJ disorders. Some may experience only mild discomfort, while others may face debilitating pain and functional limitations. Seeking prompt medical attention and working closely with a healthcare provider is crucial in determining the appropriate course of treatment, including the potential need for TMJ surgery.
Diagnosing TMJ disorders
Accurately diagnosing TMJ disorders is essential in determining the appropriate course of treatment, including the potential need for surgical intervention. Healthcare providers, such as dentists, oral and maxillofacial surgeons, and physical therapists, use a combination of clinical examinations, imaging studies, and diagnostic tests to assess the underlying cause and severity of TMJ issues.
The initial diagnostic process typically begins with a comprehensive physical examination of the jaw, face, and surrounding areas. During this examination, the healthcare provider will assess the range of motion, joint sounds, and any tenderness or pain upon palpation of the temporomandibular joint and surrounding muscles. They may also ask the patient to open and close their mouth, move their jaw from side to side, or perform other specific movements to evaluate the joint’s function.
In addition to the physical examination, healthcare providers may order various imaging tests to obtain a more detailed view of the temporomandibular joint and surrounding structures. These tests may include:
- X-rays: Provide a basic assessment of the joint’s structure and any visible abnormalities.
- CT (Computed Tomography) scans: Offer a more detailed, three-dimensional view of the joint, allowing for the identification of structural issues or changes.
- MRI (Magnetic Resonance Imaging): Helps to evaluate the soft tissues, such as the joint disc and surrounding muscles, and detect any internal derangements or inflammation.
- Arthroscopy: A minimally invasive procedure that allows the healthcare provider to visually inspect the inside of the joint using a small camera inserted through a small incision.
In some cases, the healthcare provider may also recommend additional diagnostic tests, such as bite registration or muscle palpation, to assess the patient’s occlusion (bite) and muscle function. These tests can provide valuable information to help determine the underlying cause of the TMJ disorder and guide the appropriate treatment plan.
By combining a thorough clinical examination with the use of advanced imaging and diagnostic techniques, healthcare providers can accurately diagnose TMJ disorders and develop a personalized treatment strategy, which may or may not include TMJ surgery, depending on the severity and specific needs of the patient.
Non-surgical treatment options for TMJ disorders
Before considering TMJ surgery, healthcare providers typically explore a variety of non-surgical treatment options to address TMJ disorders. These conservative approaches aim to alleviate symptoms, improve joint function, and potentially avoid the need for more invasive interventions.
One of the most common non-surgical treatments for TMJ disorders is the use of oral appliances or splints. These custom-made devices are designed to fit over the teeth and help reposition the jaw, reducing strain on the temporomandibular joint. Splints can also protect the teeth from grinding and clenching, which can exacerbate TMJ issues.
Physical therapy is another important non-surgical approach to managing TMJ disorders. A physical therapist can develop a personalized treatment plan that may include a combination of exercises, massage, and other modalities to improve joint mobility, reduce muscle tension, and alleviate pain. These techniques can help strengthen the muscles supporting the jaw and promote proper joint function.
Medication management can also play a role in the non-surgical treatment of TMJ disorders. Healthcare providers may prescribe over-the-counter or prescription pain medications, anti-inflammatory drugs, or muscle relaxants to help reduce inflammation, ease discomfort, and improve the patient’s ability to participate in other forms of treatment, such as physical therapy.
In some cases, healthcare providers may recommend lifestyle modifications to address TMJ disorders. These may include changes in diet to avoid hard or chewy foods that can aggravate the joint, stress management techniques to reduce muscle tension, and the use of hot or cold compresses to alleviate pain and inflammation.
It is important to note that the effectiveness of non-surgical treatments can vary depending on the individual and the severity of their TMJ disorder. In cases where conservative approaches fail to provide adequate relief or the condition significantly impairs the patient’s quality of life, healthcare providers may consider TMJ surgery as a potential treatment option.

When is TMJ surgery necessary?
While non-surgical treatments are often the first line of defense against TMJ disorders, there are certain circumstances when TMJ surgery may be necessary. Understanding the indicators for TMJ surgery can help individuals make informed decisions about their treatment options and seek the appropriate medical care.
One of the primary reasons for considering TMJ surgery is the failure of conservative treatments to provide sufficient relief. If a patient has undergone a comprehensive course of non-surgical interventions, such as physical therapy, oral appliances, and medication management, but continues to experience persistent and debilitating symptoms, TMJ surgery may be recommended as the next step.
Another indication for TMJ surgery is the presence of severe structural abnormalities or damage within the temporomandibular joint. This can include conditions such as joint degeneration, disc displacement, or developmental issues that cannot be adequately addressed through non-surgical means. In these cases, surgical intervention may be necessary to restore proper joint function and alleviate pain.
TMJ surgery may also be considered for individuals who experience significant limitations in their ability to perform daily activities due to their TMJ disorder. If the condition severely restricts the patient’s ability to chew, speak, or open their mouth, and these limitations significantly impact their quality of life, TMJ surgery may be a viable option to improve their functional capacity.
Additionally, TMJ surgery may be recommended for patients who exhibit signs of progressive joint damage or degeneration, as early intervention can help prevent further deterioration and potentially more complex surgical procedures in the future. Healthcare providers closely monitor the progression of TMJ disorders and may suggest surgical options to address the issue before it becomes more severe.
It is important to note that the decision to undergo TMJ surgery is a highly personalized one and should be made in close consultation with a qualified oral and maxillofacial surgeon. They will carefully evaluate the patient’s individual circumstances, weigh the potential benefits and risks, and develop a comprehensive treatment plan that addresses the specific needs and goals of the patient.
Types of TMJ surgery
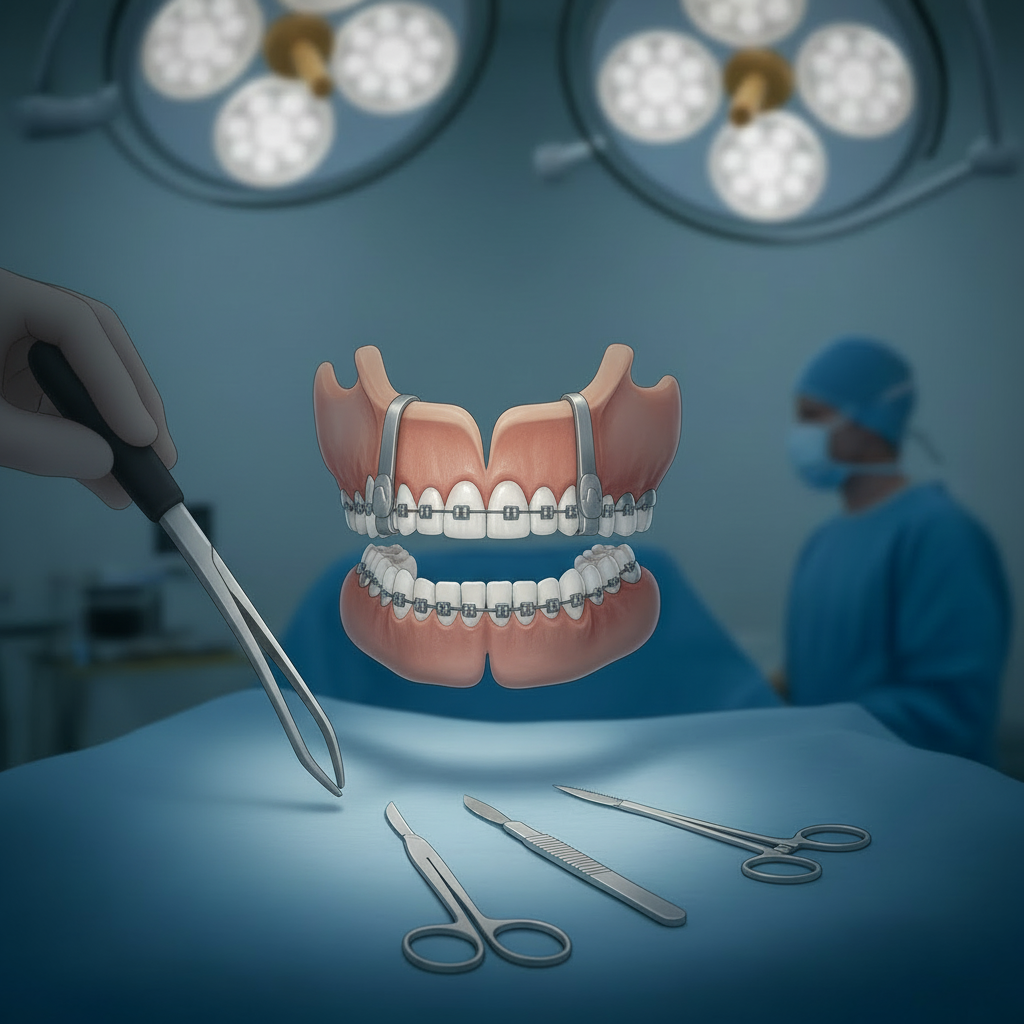
When TMJ surgery is deemed necessary, there are several different surgical options available to address the underlying issues and alleviate the patient’s symptoms. The choice of surgical approach depends on the specific nature and severity of the TMJ disorder, as well as the healthcare provider’s expertise and the patient’s preferences.
One of the most common TMJ surgical procedures is arthrocentesis, which is a minimally invasive technique. During this procedure, the healthcare provider inserts a small needle into the temporomandibular joint and flushes the joint with a saline solution to remove any debris or inflammatory byproducts that may be contributing to the patient’s discomfort. Arthrocentesis is often used as a first-line surgical intervention for TMJ disorders and can provide relief in some cases.
Another minimally invasive surgical option is arthroscopy, which involves the insertion of a small camera (arthroscope) into the temporomandibular joint through a small incision. This allows the healthcare provider to visually inspect the joint and, if necessary, perform minor surgical procedures, such as removing damaged tissue or repairing joint structures. Arthroscopic surgery is often considered a less invasive alternative to open-joint surgery, with a potentially faster recovery time.
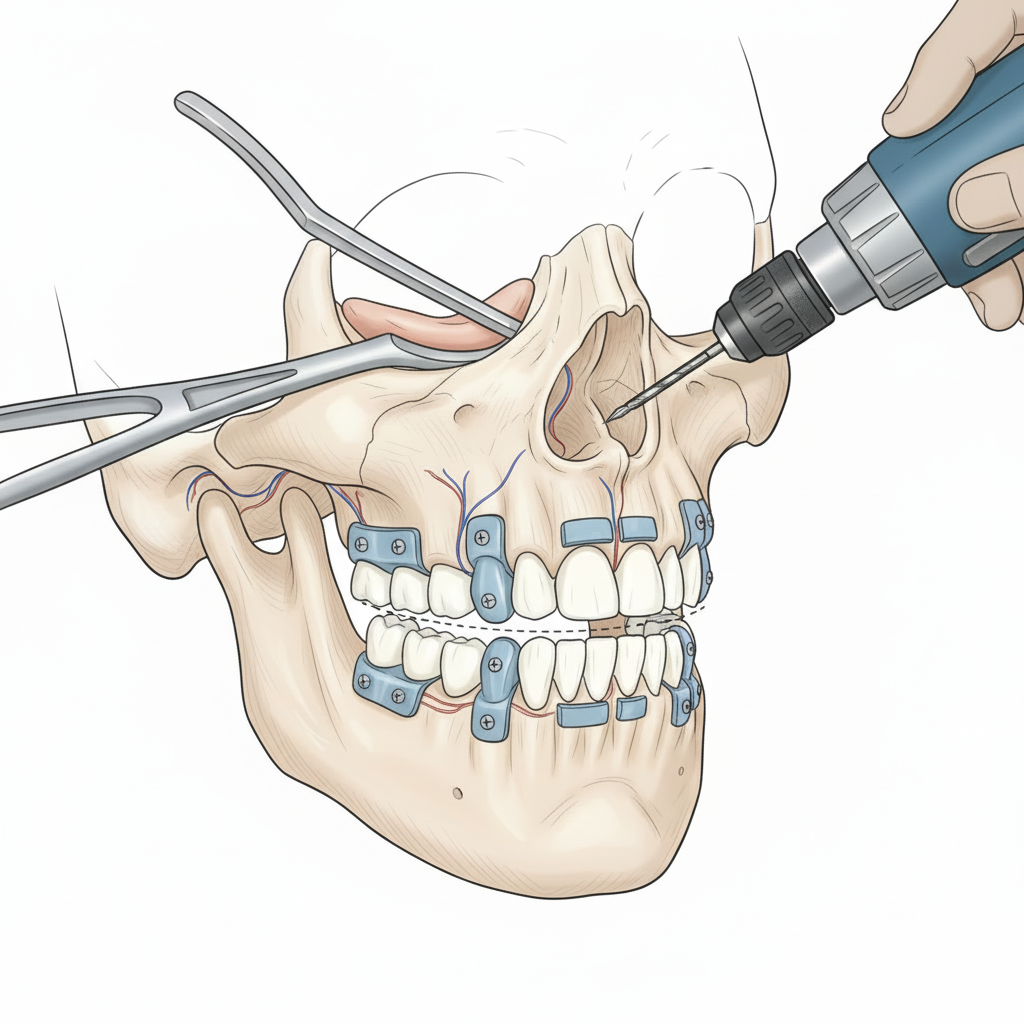
For more complex or severe TMJ issues, open-joint surgery may be recommended. This type of procedure involves making a larger incision to directly access and address the temporomandibular joint. Open-joint surgeries can include procedures such as disc repositioning, joint replacement, or joint reconstruction. These more extensive surgical interventions are typically reserved for cases where the joint has sustained significant damage or the patient’s symptoms have not responded to less invasive treatments.
In some cases, healthcare providers may recommend a combination of surgical techniques to address the patient’s specific needs. For example, they may perform an arthrocentesis or arthroscopy to assess the joint and then proceed with a more comprehensive open-joint surgery if necessary.
Regardless of the specific surgical approach, it is crucial for patients to work closely with their healthcare provider to understand the potential risks, benefits, and recovery process associated with each type of TMJ surgery. This collaboration will help ensure that the chosen treatment plan aligns with the patient’s individual goals and preferences.
Risks and complications of TMJ surgery
While TMJ surgery can be an effective solution for individuals with severe and chronic TMJ disorders, it is important to be aware of the potential risks and complications associated with these procedures. Understanding the potential downsides of TMJ surgery can help patients make an informed decision about their treatment options.
One of the primary risks of TMJ surgery is the potential for postoperative pain and discomfort. Even with advanced surgical techniques, patients may experience some level of pain, swelling, and stiffness in the jaw and surrounding areas following the procedure. Healthcare providers typically prescribe pain medication and recommend physical therapy to help manage these symptoms during the recovery process.
Another potential complication of TMJ surgery is the risk of nerve damage. The temporomandibular joint is located in close proximity to several nerves, including the facial nerve, which controls the muscles of the face. While healthcare providers take great care to avoid damaging these delicate structures, there is a small risk of temporary or permanent nerve injury, which can lead to issues such as facial paralysis or numbness.
In some cases, TMJ surgery may not achieve the desired outcome, and the patient may continue to experience persistent symptoms or even a worsening of their condition. This can be due to a variety of factors, including the complexity of the underlying issue, individual variations in healing, or the development of new complications. In such instances, additional surgical or non-surgical interventions may be necessary.
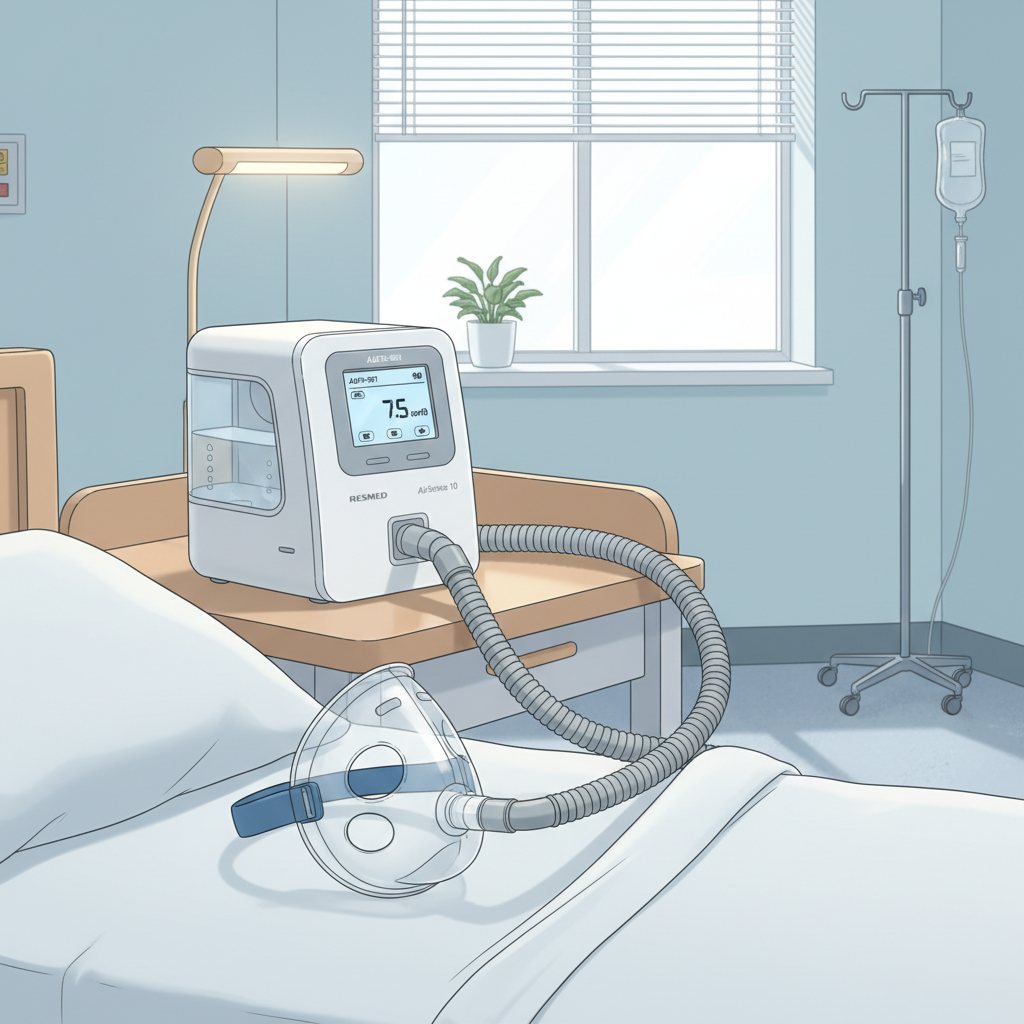
Other potential risks associated with TMJ surgery include infection, bleeding, and the general risks associated with anesthesia and any surgical procedure, such as blood clots or respiratory complications. Patients with underlying health conditions, such as cardiovascular disease or diabetes, may be at a higher risk of experiencing these complications.
It is crucial for patients to have a thorough discussion with their healthcare provider about the specific risks and potential complications associated with their recommended TMJ surgery. This information, along with a clear understanding of the expected outcomes and recovery process, will help patients make an informed decision about their treatment and set realistic expectations for the surgical intervention.

Recovery and aftercare following TMJ surgery
Recovering from TMJ surgery can be a gradual process, and the timeline for healing and regaining full function of the jaw can vary depending on the type of procedure performed and the individual’s response to treatment. Understanding the recovery process and the necessary aftercare can help patients prepare for and navigate the post-surgical phase effectively.
Immediately following the surgery, patients can expect to experience some discomfort, swelling, and limited jaw movement. Healthcare providers will typically prescribe pain medication and recommend the use of ice packs to help manage these initial symptoms. Patients may also be advised to follow a soft or liquid diet in the early stages of recovery to avoid excessive chewing and further irritation of the surgical site.
As the initial swelling and discomfort subside, patients will begin to engage in physical therapy exercises designed to restore jaw mobility, strength, and function. These exercises may include gentle stretching, massage, and the use of specialized devices to gradually increase the range of motion. The physical therapist will work closely with the patient to develop a personalized rehabilitation plan and monitor their progress throughout the recovery process.
In addition to physical therapy, patients may also be required to wear a custom-made oral appliance, such as a splint or bite guard, to help protect the jaw and prevent further strain on the temporomandibular joint. These devices are typically worn for an extended period, often several months, to ensure proper healing and joint stabilization.
The overall recovery timeline can vary significantly, depending on the type of TMJ surgery performed and the individual’s response to treatment. In general, patients can expect to resume normal daily activities and a regular diet within a few weeks to a few months, with the full recovery process taking several months to a year or more in some cases.
It is essential for patients to follow their healthcare provider’s instructions and attend all scheduled follow-up appointments during the recovery period. This allows for the monitoring of progress, the identification of any potential complications, and the adjustment of the rehabilitation plan as needed. Adherence to the recommended aftercare regimen can significantly improve the chances of a successful outcome and a return to normal jaw function.
Conclusion: Is TMJ surgery right for you?
If you are struggling with chronic and debilitating TMJ disorders, you may be wondering if TMJ surgery is the right solution for you. While the decision to undergo surgery is a highly personal one, this comprehensive guide has provided you with the information you need to make an informed choice about your treatment options.
We have explored the various causes and symptoms of TMJ disorders, the diagnostic process, and the range of non-surgical treatment approaches that may be considered before resorting to surgery. Understanding these factors is crucial in determining whether TMJ surgery is necessary and the appropriate timing for such an intervention.
When conservative treatments fail to provide adequate relief or the TMJ disorder significantly impairs an individual’s quality of life, TMJ surgery may be the best course of action. We have discussed the different types of TMJ surgical procedures, from minimally invasive arthrocentesis and arthroscopy to more complex open-joint surgeries, each tailored to address specific issues related to the temporomandibular joint.