Are you considering jaw surgery but unsure about the recovery process? Understanding the timeline of jaw surgery rehabilitation is essential for a smooth and successful recovery. With a maximum of 160 words, we’ll guide you through the journey to full recovery.
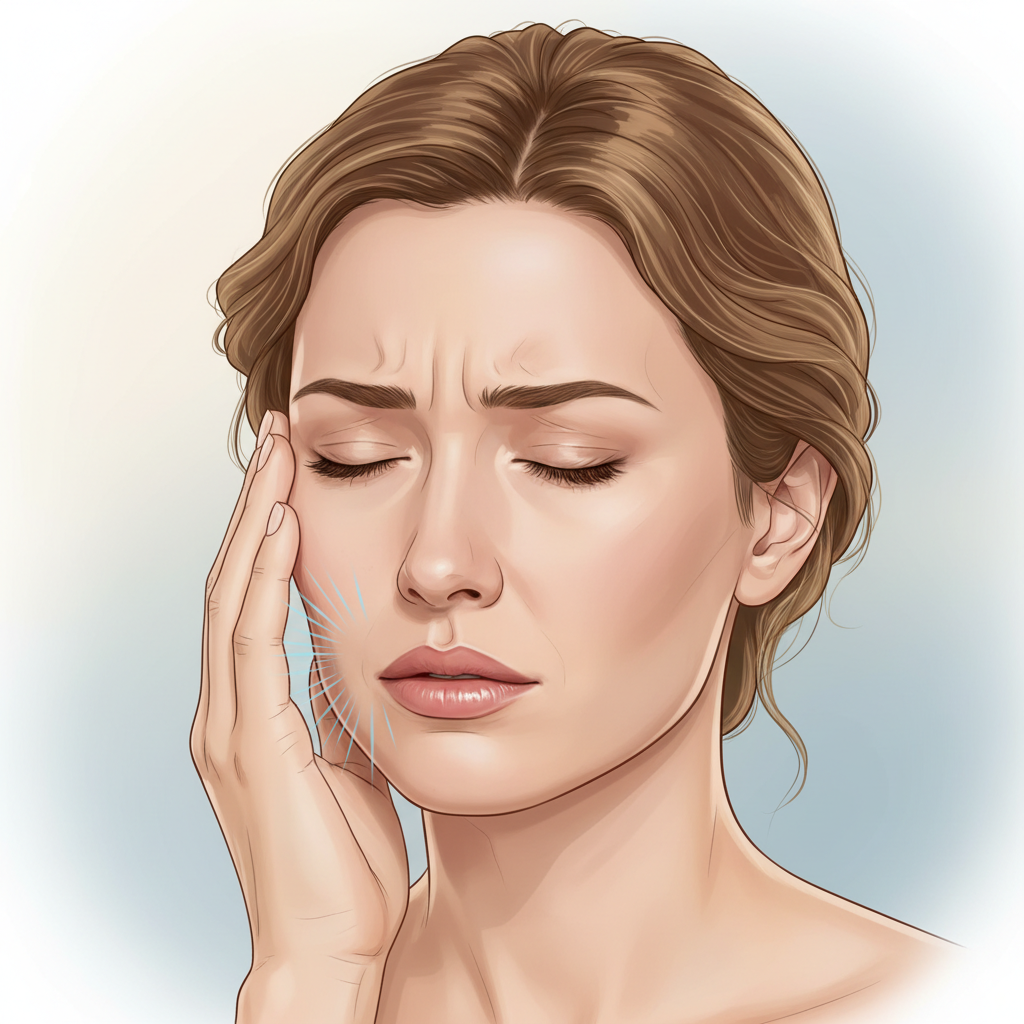
After undergoing jaw surgery, you might experience swelling and discomfort for the first few days. Over the next week or two, the discomfort should gradually subside as your body starts healing. It’s not uncommon to have difficulty speaking and eating during this initial recovery stage.
As time progresses, you’ll notice significant improvements in your ability to open and close your mouth. Your jaw muscles will start adapting to the new position, allowing you to regain normal function. Physiotherapy may be recommended to assist in strengthening the muscles and improving mobility.
Full recovery varies for each individual but generally takes several weeks to a few months. It’s important to follow your surgeon’s guidance regarding diet, oral hygiene, and activity restrictions. By understanding the timeline and being patient with the healing process, you’ll be well on your way to restoring jaw function and enjoying an improved quality of life after surgery.
The importance of jaw surgery rehabilitation
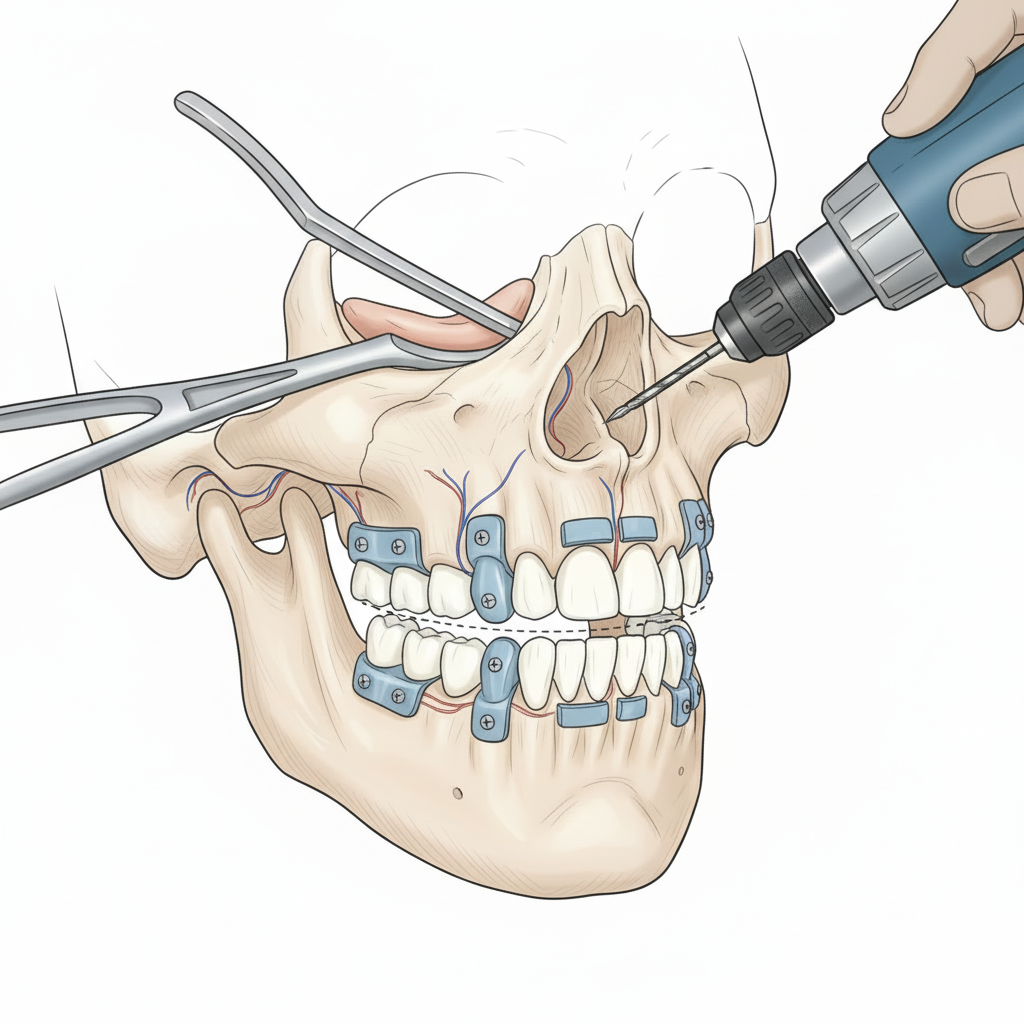
Jaw surgery, also known as orthognathic surgery, is a complex procedure that involves reshaping the jaw bones to correct misalignment, improve function, and enhance facial aesthetics. While the surgical intervention itself is critical, the rehabilitation process that follows is equally important for a successful outcome.
Proper rehabilitation is essential for regaining full jaw function, reducing the risk of complications, and ensuring a smooth recovery. During the rehabilitation phase, patients work closely with a team of healthcare professionals, including surgeons, physical therapists, and dental specialists, to restore normal jaw movement, strength, and mobility.
Without a comprehensive rehabilitation program, patients may experience ongoing challenges, such as difficulty chewing, speaking, or swallowing, as well as potential complications like TMJ (temporomandibular joint) dysfunction, muscle imbalances, or even a relapse of the original jaw misalignment. By prioritizing rehabilitation, patients can maximize the benefits of their jaw surgery and achieve their desired long-term outcomes.
Preparing for jaw surgery rehabilitation
Before undergoing jaw surgery, it is essential for patients to understand the rehabilitation process and prepare themselves both physically and mentally. This preparation can significantly improve the overall recovery experience and increase the chances of a successful outcome.
One of the key steps in preparation is to engage in pre-surgical physical therapy. A physical therapist can work with the patient to assess their current jaw function, strength, and range of motion, and then develop a tailored exercise program to help prepare the body for the upcoming surgery and rehabilitation. This might include exercises to strengthen the jaw muscles, improve flexibility, and promote overall physical conditioning.
Additionally, patients should familiarize themselves with the specific rehabilitation plan outlined by their surgical team. This includes understanding the timeline of recovery, the types of exercises and activities they will need to perform, and any dietary or lifestyle modifications they may need to make. By being proactive and engaging in this preparation, patients can feel more confident and empowered throughout the rehabilitation process.
Immediate post-surgery care and recovery
Immediately following jaw surgery, patients can expect to experience a period of discomfort, swelling, and limited jaw mobility. This initial recovery phase is crucial, as it lays the foundation for the subsequent rehabilitation process.
During the first few days after the surgery, patients will typically be monitored closely by their healthcare team to ensure proper healing and manage any pain or swelling. Pain medication may be prescribed, and patients may be advised to apply ice packs to the affected areas to reduce inflammation.
In the early stages of recovery, patients may also be required to follow a liquid or soft food diet, as chewing and swallowing solid foods can be challenging. Oral hygiene routines may need to be modified, and patients may be instructed to avoid certain activities, such as strenuous exercise, to allow the jaw to heal properly.
As the initial swelling and discomfort begin to subside, patients will gradually be able to open their mouths more and engage in gentle exercises to promote jaw mobility. This is where the rehabilitation process truly begins, with the guidance of a physical therapist or other healthcare professionals.
Early-stage rehabilitation exercises
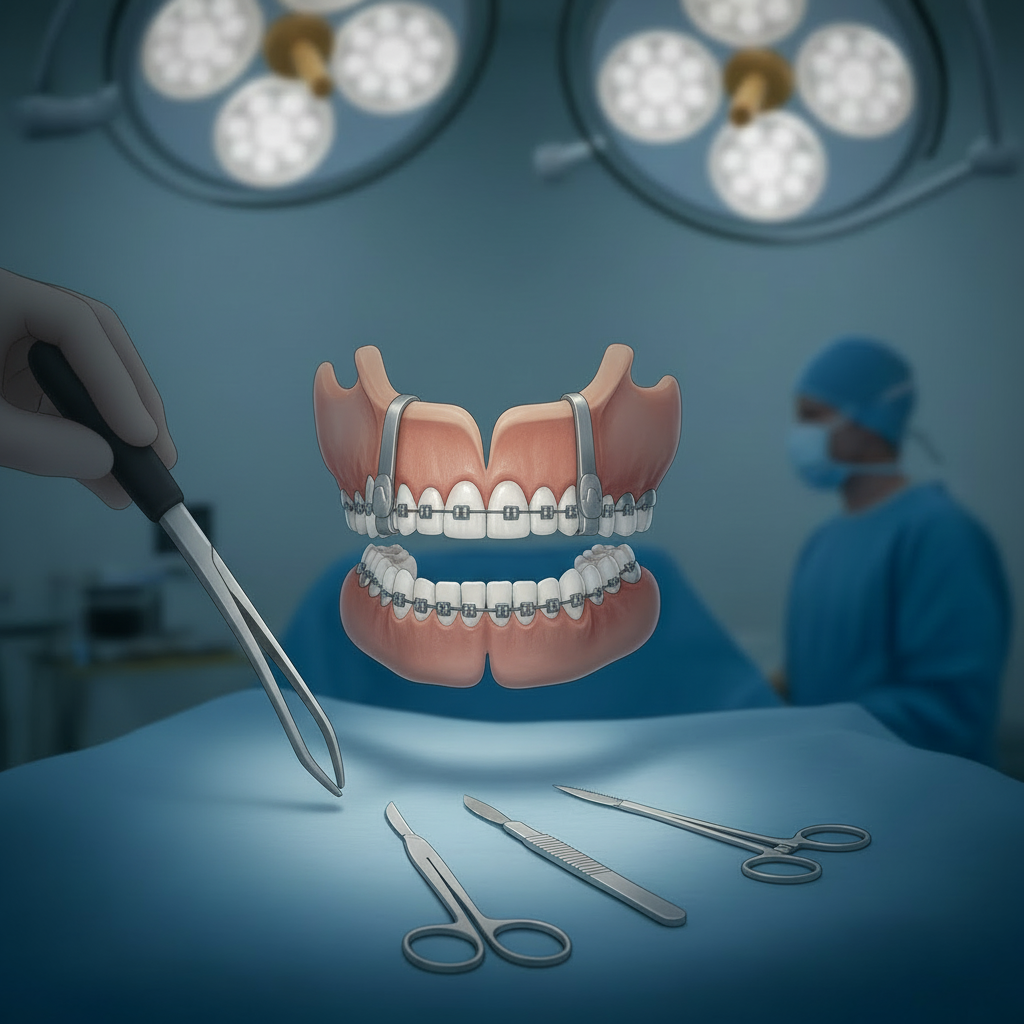
In the early stages of rehabilitation, the primary focus is on regaining basic jaw function and mobility. Patients will typically work with a physical therapist to perform a series of gentle exercises and stretches designed to gently move the jaw and surrounding muscles.
One common exercise during this phase is the “passive jaw opening” exercise, where the therapist manually opens the patient’s mouth to a comfortable range, holding it for a few seconds before slowly closing it. This helps to gradually increase the jaw’s range of motion and prevent the formation of scar tissue that could limit mobility.
Other exercises may include gentle jaw movements, such as side-to-side or up-and-down motions, as well as exercises to strengthen the muscles responsible for opening and closing the jaw. Patients may also be instructed to perform self-massage techniques to help reduce muscle tension and improve circulation.
Throughout this early stage, it is crucial for patients to follow their rehabilitation plan closely and communicate any concerns or discomfort to their healthcare team. Patience and consistency are key, as the rehabilitation process can be gradual and require regular practice.
Mid-stage rehabilitation exercises
As the initial healing process progresses, patients will move into the mid-stage of rehabilitation, where the focus shifts to more intensive exercises and activities to restore full jaw function.
During this phase, patients may be introduced to exercises that challenge the jaw muscles more, such as resisted opening and closing exercises using rubber bands or other resistance devices. These exercises help to strengthen the muscles and improve their coordination, which is essential for regaining normal chewing and speaking abilities.
Patients may also be encouraged to engage in exercises that simulate everyday activities, such as biting on a tongue depressor or chewing on a soft, chewy food item. These exercises help to retrain the jaw muscles and prepare the patient for a return to a normal diet and lifestyle.
In addition to jaw-specific exercises, patients may also be introduced to more general physical therapy exercises, such as neck and shoulder stretches, to address any related muscle imbalances or restrictions that could be impacting jaw function.
Throughout the mid-stage rehabilitation, patients will work closely with their physical therapist to monitor progress, adjust the exercise program as needed, and ensure that they are on track to achieve their rehabilitation goals.
Late-stage rehabilitation exercises
As the patient progresses through the rehabilitation process, the focus will shift to more advanced exercises and activities designed to fully restore jaw function and prepare the patient for a return to normal daily activities.
During the late-stage rehabilitation, patients may be introduced to exercises that challenge the jaw in more dynamic and functional ways. This might include exercises that simulate chewing, biting, or speaking, such as biting on different textures of food or practicing articulation exercises.
Patients may also be encouraged to engage in more complex, multi-joint exercises that integrate the jaw with other parts of the body, such as exercises that involve turning the head while opening and closing the mouth. These exercises help to improve overall coordination and neuromuscular control, which is essential for regaining full jaw function.
In addition to the physical exercises, patients may also be guided through activities that simulate real-world scenarios, such as practicing eating a meal or engaging in conversation. This helps to ensure that the patient is prepared to transition back to their normal routine and lifestyle.
Throughout the late-stage rehabilitation, the healthcare team will closely monitor the patient’s progress and make any necessary adjustments to the rehabilitation plan to ensure a successful outcome.
Foods to eat during jaw surgery rehabilitation
During the recovery and rehabilitation process following jaw surgery, it is essential for patients to pay close attention to their dietary needs and make appropriate adjustments to support the healing and recovery of the jaw.
In the immediate aftermath of the surgery, patients will typically be advised to follow a liquid or soft food diet, as chewing and swallowing solid foods can be challenging and potentially painful. This may include items such as soups, smoothies, yogurt, and pureed or mashed fruits and vegetables.
As the patient progresses through the rehabilitation process and regains more jaw mobility and strength, the diet can gradually be expanded to include soft, easy-to-chew foods, such as mashed potatoes, cooked pasta, scrambled eggs, and well-cooked meats that have been cut into small pieces.
It is important to avoid hard, crunchy, or chewy foods, as these can put excessive stress on the jaw and potentially cause discomfort or delay the healing process. Patients should also be mindful of the temperature of their food, as extremely hot or cold items can also be uncomfortable.
Throughout the rehabilitation process, patients should focus on consuming a balanced, nutrient-rich diet that supports the body’s healing and recovery. This may include foods that are high in protein, vitamins, and minerals, such as lean meats, fish, eggs, dairy products, fruits, and vegetables.
By carefully selecting and preparing appropriate foods during the rehabilitation period, patients can support the healing of their jaw, promote muscle recovery, and ultimately achieve a successful outcome from their jaw surgery.
Potential challenges and how to overcome them
While the rehabilitation process following jaw surgery is crucial for a successful outcome, patients may face various challenges along the way. Understanding these potential challenges and having strategies to overcome them can help ensure a smooth and efficient recovery.
One common challenge is managing pain and discomfort during the rehabilitation exercises. Patients may experience soreness, stiffness, or even pain in the jaw and surrounding areas as they work to regain mobility and strength. To address this, patients should work closely with their healthcare team to ensure they are managing pain effectively, whether through the use of over-the-counter medications, ice packs, or other pain management techniques.
Another challenge may be maintaining motivation and adherence to the rehabilitation program, as the process can be lengthy and require consistent effort. Patients should work with their healthcare team to set realistic goals, celebrate small victories, and find ways to make the exercises and activities enjoyable, such as by incorporating music or engaging in social activities with other jaw surgery patients.
Some patients may also experience difficulties with speech and swallowing, particularly in the early stages of rehabilitation. This can be addressed through specialized speech therapy, which can help patients relearn and retrain the muscles involved in these functions. Patients should be patient and persistent, as progress in these areas may be gradual.
Finally, some patients may face challenges with the emotional and psychological aspects of the recovery process, such as feelings of frustration, anxiety, or depression. It is important for patients to seek support from their healthcare team, family, and friends, and to consider engaging in counseling or other mental health resources if needed.
By being proactive, communicating openly with their healthcare team, and having a positive mindset, patients can overcome these potential challenges and successfully navigate the rehabilitation process following jaw surgery.
Final thoughts on the timeline of jaw surgery rehabilitation
Undergoing jaw surgery is a significant undertaking, but with proper rehabilitation, patients can achieve a successful outcome and restore full jaw function. The timeline of jaw surgery rehabilitation is a gradual and multifaceted process, requiring patience, dedication, and the support of a comprehensive healthcare team.
From the immediate post-surgery care and recovery to the early, mid, and late-stage rehabilitation exercises, each phase plays a crucial role in the overall rehabilitation process. By understanding the timeline and actively engaging in the rehabilitation program, patients can maximize their chances of regaining normal jaw movement, strength, and function.
Throughout the rehabilitation journey, patients should remain vigilant about their dietary needs, addressing any challenges that arise, and maintaining a positive mindset. By doing so, they can overcome obstacles and achieve their desired outcome, ultimately improving their quality of life and overall well-being.
Ultimately, the timeline of jaw surgery rehabilitation is a personalized experience, and the specific duration and progression may vary for each individual. However, by following the guidance of their healthcare team and remaining committed to the rehabilitation process, patients can look forward to a full recovery and a renewed sense of confidence and functionality in their daily lives.