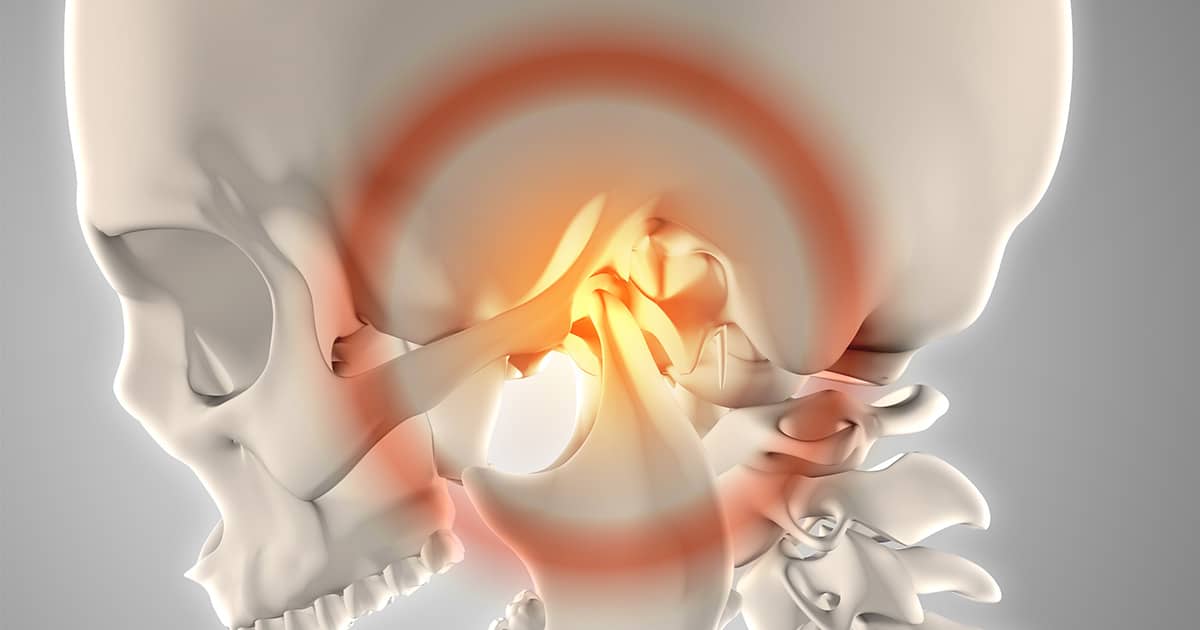
Dr. Wolford treats one of the most common types of TMJ disorder, a displaced articular disc. This occurs when a disc slips out of its proper position.
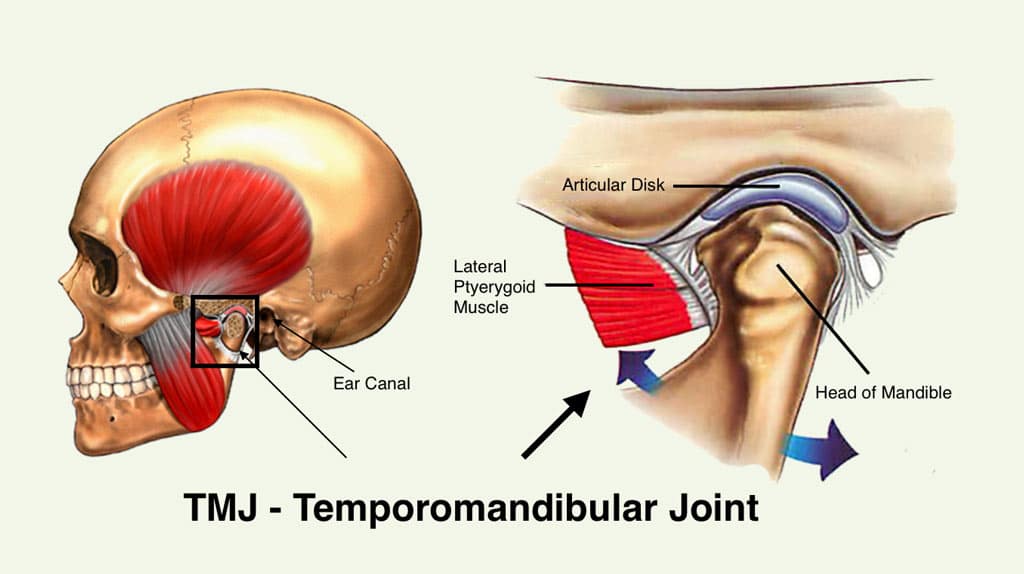
Comprised of numerous bones, muscles, tendons, and other components, the jaw is one of the most complex joints in the body. This is understandable, as the jaw has to move in multiple directions and planes to chew food properly and facilitate speech.
However, all of those parts present ample opportunity for problems to develop. A collection of jaw issues known as temporomandibular joint (TMJ) disorders can cause significant discomfort and other problematic symptoms for patients.
Displaced Articular Disc Treatment
In treating TMJ disorders, a TMJ specialist must first diagnose the specific cause of the patient’s pain. The most common type of TMJ disorder is a displaced articular disc. This occurs when a disc slips out of its proper position. A TMJ specialist can recommend a number of different treatment options that can be effective for a particular case of TMJ disorder.
For example, when a displaced articular disc is involved, an oral surgeon may need to place a device known as a Mitek Anchor to stabilize the disc in its correct location.
A congenital defect or uneven developmental rates of the upper and lower jaws that result in TMJ disorders may also necessitate a surgical intervention.
On the other hand, some TMJ cases can be managed with pain medication or stress management techniques. If the cause of the TMJ disorder is not a structural defect within the jaw, the oral surgeon can consider less invasive treatment options.
In addition to the characteristic jaw pain, various other symptoms may indicate TMJ disorder. If you notice any of the following, schedule an evaluation with a TMJ specialist:
- Clicking or popping noises while opening or closing the jaw
- “Locking” of jaw in place
- Headaches
- Ear pain/aches
- Pain in the neck and shoulders
- Difficulty chewing
- Dizziness
TMJ disorders are generally treatable, meaning patients don’t have to endure the pain forever. If you have questions or want to schedule an appointment, don’t hesitate to contact Dr. Larry Wolford’s office using our online contact form or call 214-828-9115.