Jaw pain, clicking sounds, and difficulty chewing are more than just minor annoyances; they can be signs of a temporomandibular joint (TMJ) disorder. These conditions affect the complex joint that connects your jaw to your skull, causing a range of uncomfortable and often painful symptoms that can disrupt daily life. While many cases can be managed with conservative treatments, some require the specialized expertise of a surgeon.
When non-surgical options are not enough, a maxillofacial surgeon plays a crucial role in diagnosing and treating complex TMJ problems. This article will delve into what TMJ disorders are, their common symptoms, and the advanced treatment options that a highly trained surgeon can provide to restore comfort and function.
What Are TMJ Disorders?
The temporomandibular joint is one of the most intricate joints in the body, acting as a sliding hinge that allows you to talk, chew, and yawn. TMJ disorders (TMD) are a group of conditions that cause pain and dysfunction in this joint and the muscles that control jaw movement.
The exact cause of a person’s TMJ disorder can be difficult to determine. According to the National Institute of Dental and Craniofacial Research (NIDCR), pain can stem from a combination of factors, such as genetics, arthritis, or a jaw injury. Some of the most common contributing factors include:
- Disc Erosion or Misalignment: The joint includes a small disc of cartilage that acts as a cushion. If this disc erodes or moves out of its proper alignment, it can cause clicking, popping, or pain. Source: Mayo Clinic
- Arthritis: Degenerative joint diseases like osteoarthritis or rheumatoid arthritis can damage the cartilage in the TMJ. Source: Cleveland Clinic
- Jaw Injury: A heavy impact to the jaw, such as from an accident or blow, can lead to dislocation or damage to the joint.
- Chronic Grinding or Clenching: Habitual teeth grinding (bruxism) can put immense pressure on the TMJ, leading to inflammation and pain. Source: WebMD
- Stress: Physical and emotional stress can cause individuals to tighten their facial and jaw muscles, contributing to TMJ pain.
Common Symptoms of TMJ Disorders
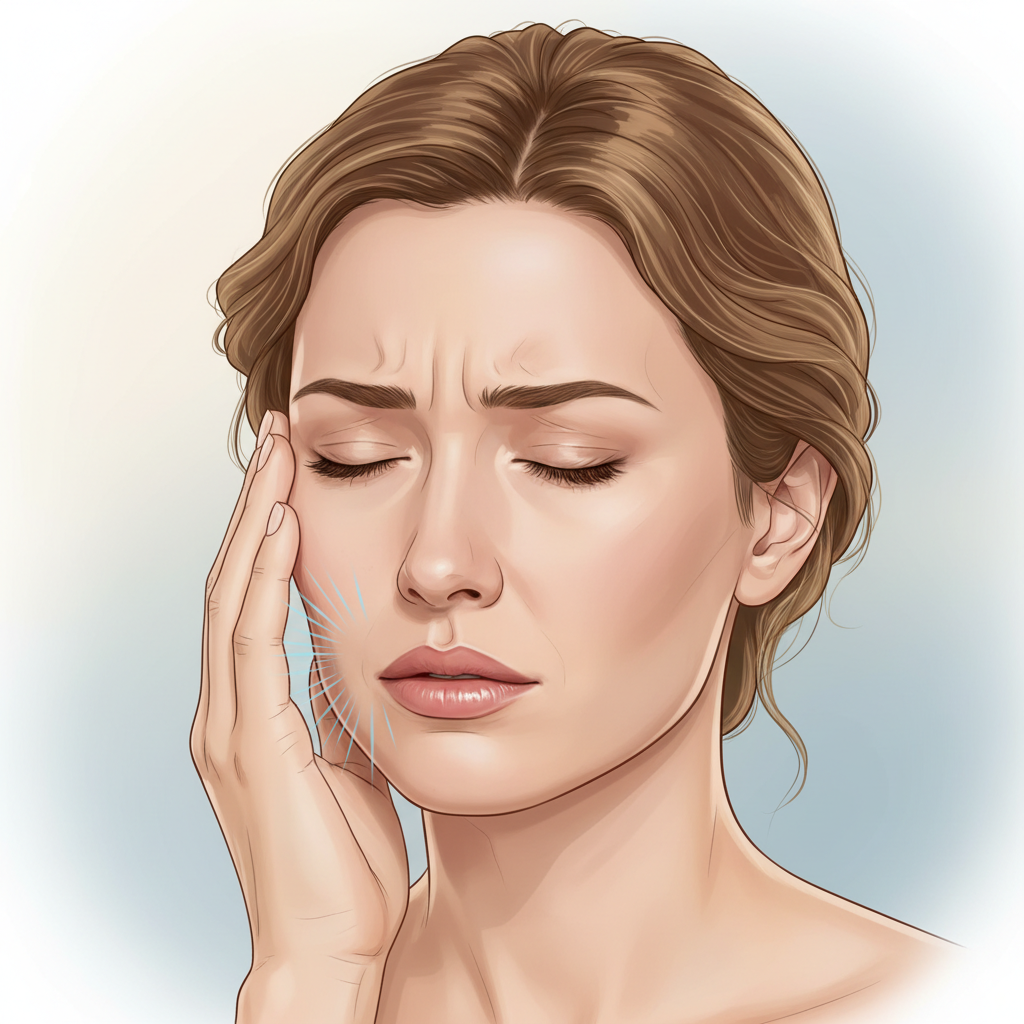
TMJ disorders can manifest in various ways, and symptoms can be temporary or last for years. Recognizing these signs is the first step toward seeking proper diagnosis and treatment. Common symptoms include:
- Pain or tenderness in the jaw, face, neck, and shoulders, especially when chewing or speaking.
- A clicking, popping, or grating sound in the jaw joint when opening or closing the mouth.
- The jaw getting “stuck” or “locked” in an open or closed position.
- Limited ability to open the mouth wide.
- A tired feeling in the face.
- Difficulty chewing or a sudden uncomfortable bite, as if the upper and lower teeth are not fitting together properly.
- Swelling on the side of the face.
- Frequent headaches or earaches.
Because these symptoms can overlap with other conditions, a thorough evaluation by a qualified healthcare professional is essential for an accurate diagnosis. Read more from Johns Hopkins Medicine.
How a Maxillofacial Surgeon Diagnoses TMJ Disorders
When you see a Maxillofacial Surgeon for TMJ-related issues, the diagnostic process is comprehensive. A surgeon will typically:
- Discuss Your Symptoms and Medical History: The evaluation starts with a detailed conversation about your pain, jaw noises, and any relevant medical history, including past injuries or conditions like arthritis.
- Perform a Physical Examination: The surgeon will observe the range of motion of your jaw, press on areas around the jaw to identify points of pain or tenderness, and listen for sounds during jaw movement.
- Utilize Advanced Imaging: To get a clear picture of the joint, imaging studies are often necessary. These may include X-rays to view the teeth and jaws, a CT scan to provide detailed images of the bones in the joint, or an MRI to reveal problems with the joint’s disc or surrounding soft tissue. Learn more about diagnostic techniques from the American Association of Oral and Maxillofacial Surgeons (AAOMS).
This detailed evaluation allows the surgeon to identify the specific cause of the disorder and develop a targeted treatment plan.
Treatment Options Offered by Maxillofacial Surgeons
Treatment for TMJ disorders typically follows a “less is more” approach, starting with conservative, non-surgical therapies. However, when pain and dysfunction persist, a maxillofacial surgeon can offer more advanced interventions.
Non-Surgical and Minimally Invasive Treatments
Before recommending surgery, a surgeon will ensure that all conservative options have been explored. These can include pain relievers, anti-inflammatories, physical therapy, or oral splints (bite guards). Source: NIDCR TMJ Treatment. If these methods fail to provide relief, a surgeon might suggest procedures such as:
- Arthrocentesis: This is a minimally invasive procedure that involves inserting small needles into the joint to irrigate it with sterile fluid. This can help wash out inflammatory byproducts and may help the jaw move more freely. Read more: Mayo Clinic – TMJ Arthrocentesis
- Injections: For some patients, corticosteroid injections into the joint can help decrease inflammation and relieve pain. In other cases, injections into the jaw muscles can help relieve pain associated with muscle tension.
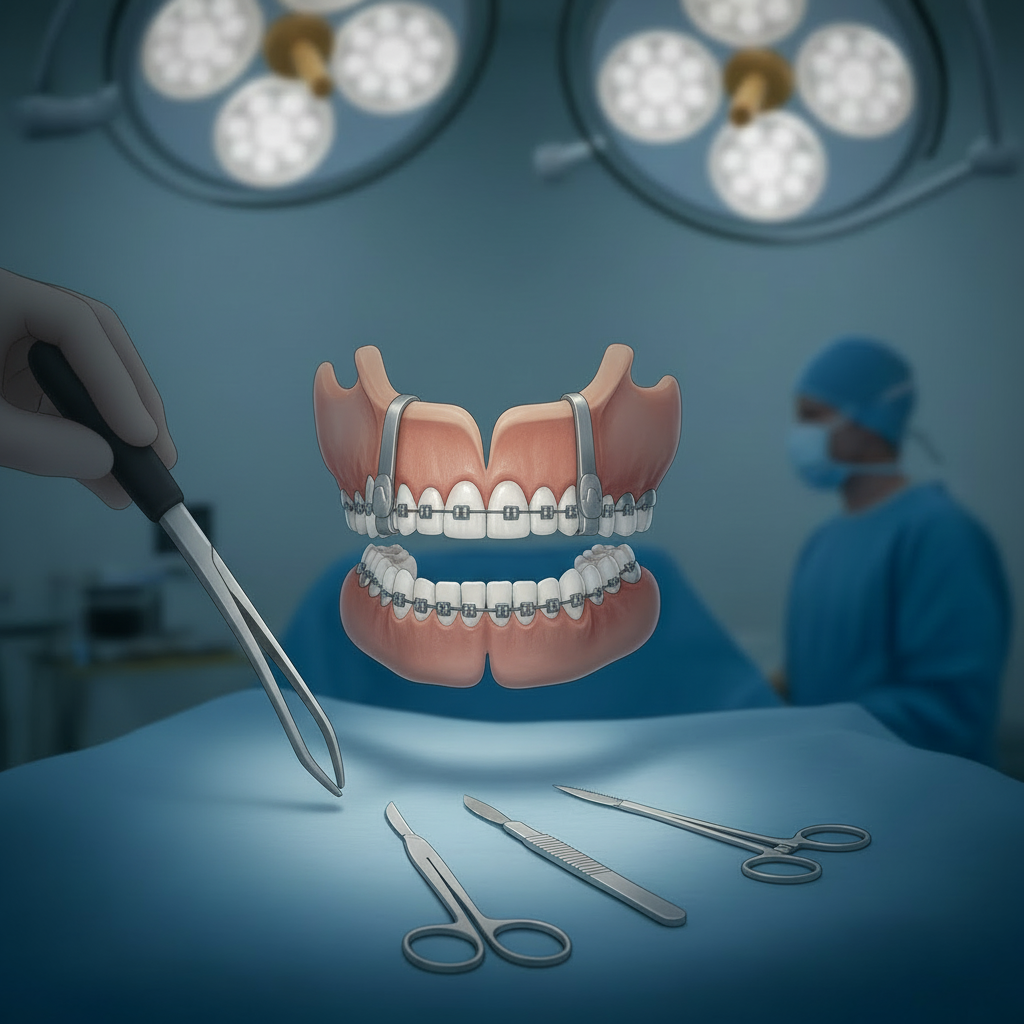
Surgical Interventions
When a clear structural problem exists within the joint or when non-surgical treatments are ineffective, surgical options may be considered. A maxillofacial surgeon is uniquely qualified to perform these complex procedures.
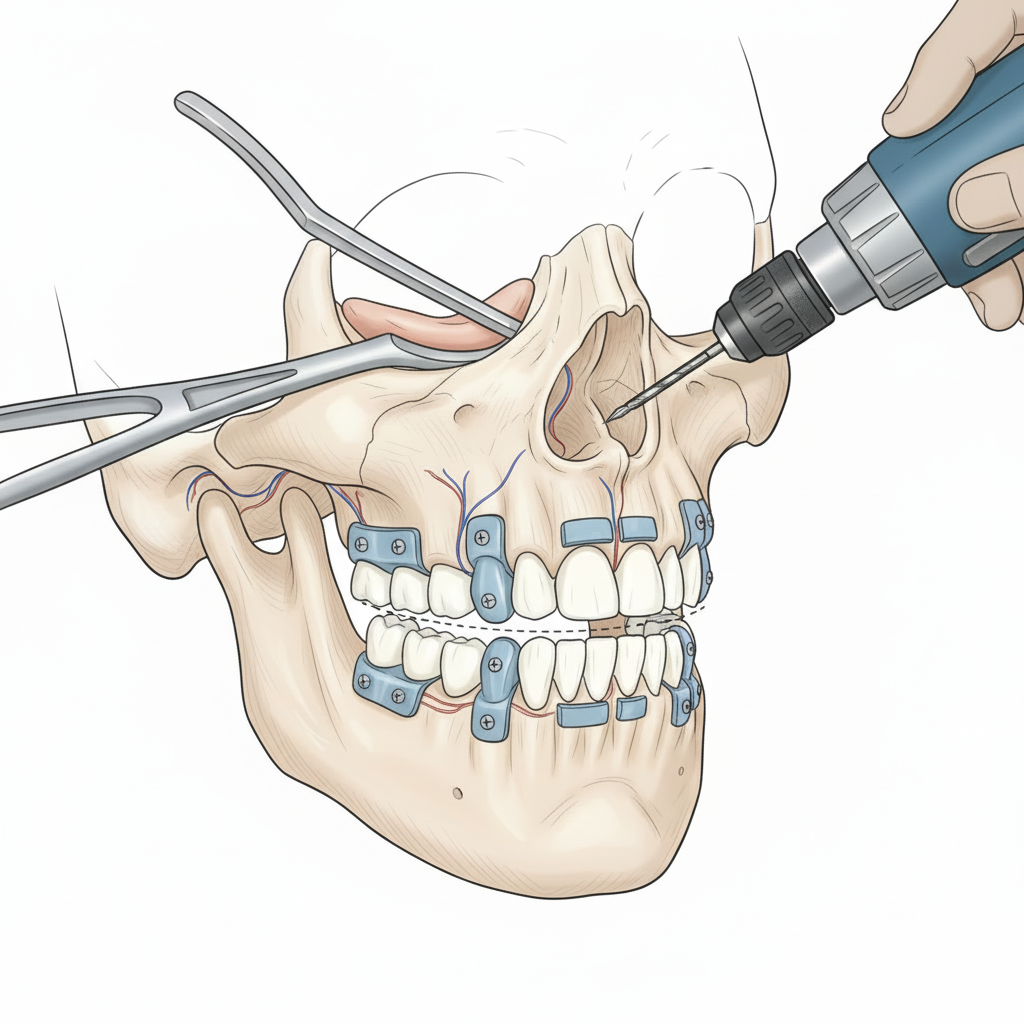
- TMJ Arthroscopy: Similar to arthroscopic procedures on knees or shoulders, this minimally invasive surgery uses a small camera (arthroscope) inserted into the joint space. This allows the surgeon to directly view the inside of the joint, remove inflamed tissue, and reposition a misaligned disc. The American Association of Oral and Maxillofacial Surgeons highlights that this procedure has a high success rate with minimal complications.
- Modified Condylotomy: This surgery is performed on the mandible (lower jawbone) rather than the joint itself. It is often recommended for patients experiencing jaw locking and may be helpful for those with internal derangement of the joint.
- Open-Joint Surgery (Arthroplasty): For more severe cases, the surgeon may need to perform an open surgery to repair or replace the joint. This procedure is reserved for patients with significant structural damage, such as worn-out bone, tumors in or around the joint, or severe scarring. The surgeon makes an incision in front of the ear to expose the joint, allowing for a full repair of the damaged components. Further reading: Cleveland Clinic – TMJ Surgery
- Total Joint Replacement: In the most advanced cases where the joint is severely degenerated and cannot be salvaged, a total TMJ replacement may be necessary. Similar to hip or knee replacements, this procedure involves replacing the damaged parts of the jaw joint with custom-made artificial implants. This can restore function and provide significant pain relief for patients with end-stage TMJ disease. See details from Johns Hopkins Medicine – TMJ Surgery.
Finding Relief and Restoring Function
Living with chronic jaw pain can be debilitating. TMJ disorders compromise your ability to eat, speak, and express yourself comfortably. A maxillofacial surgeon offers a level of expertise that is critical for diagnosing the root cause of complex TMJ problems and providing effective, long-lasting solutions. By moving from conservative therapies to advanced surgical interventions, these specialists can help patients find lasting relief, restore proper jaw function, and dramatically improve their quality of life.