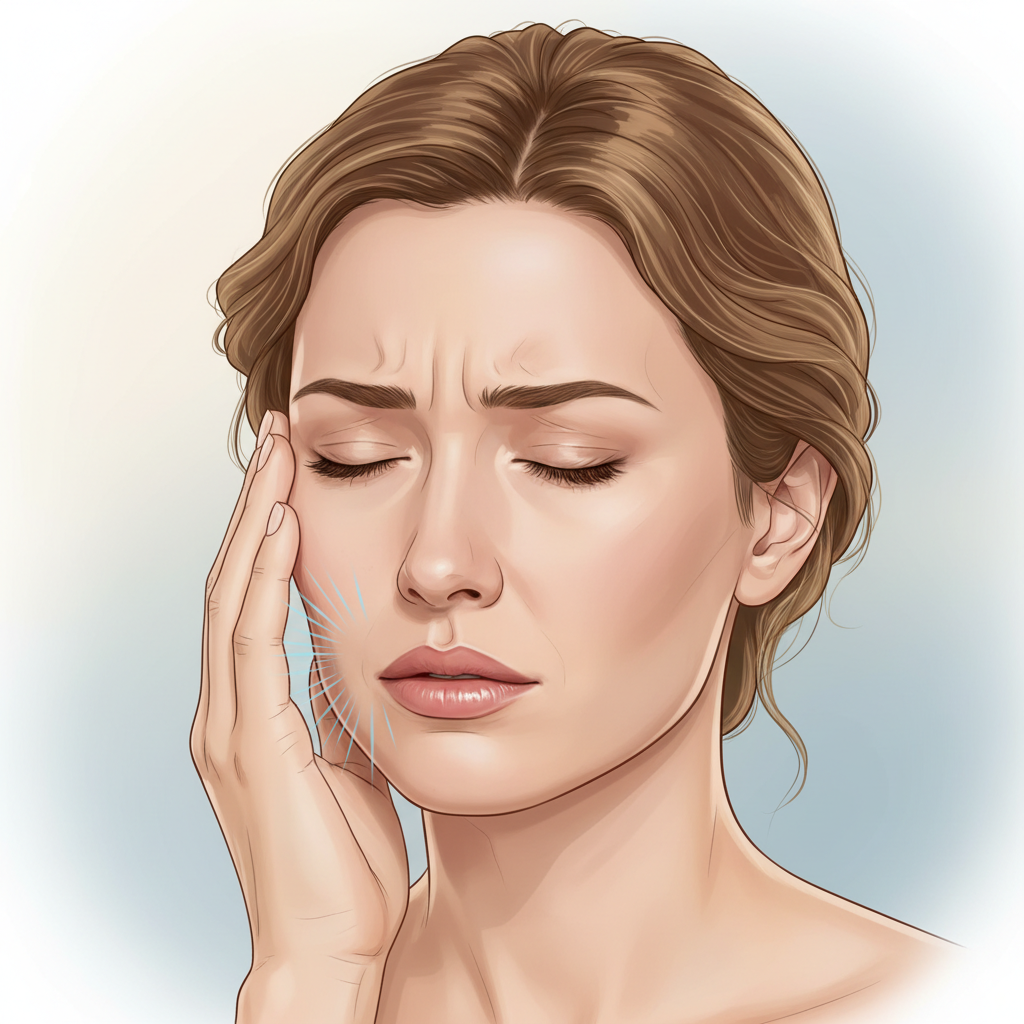
A persistent headache can disrupt your entire day, making it difficult to focus, work, or even relax. While many people attribute chronic headaches to stress, eye strain, or migraines, the root cause is sometimes found in an unexpected place: your jaw. The intricate system of muscles, nerves, and joints that allows you to chew and speak can become a significant source of head pain when something is wrong. This connection is often overlooked, leaving many to suffer without understanding the true origin of their discomfort.
Temporomandibular joint (TMJ) disorders are a group of conditions that affect the jaw joint and the muscles controlling jaw movement. The pain they generate is not always confined to the jaw itself. In fact, one of the most common symptoms is a recurring headache that seems to have no other explanation. Understanding how jaw dysfunction can trigger head pain is the first step toward finding a lasting solution. Experts like Dr. Larry Wolford specialize in diagnosing and treating these complex cases, offering relief to patients who have struggled for years.
How Do TMJ Disorders Cause Headaches?
The temporomandibular joint connects your jawbone to your skull, just in front of your ears. It is one of the most complex joints in the body, responsible for both hinge and sliding motions. This joint works in close partnership with a network of muscles and nerves in your head, face, and neck. When the TMJ is not functioning correctly, it creates a chain reaction that can lead to significant pain.
There are several ways TMJ disorders can trigger headaches:
- Muscle Tension and Fatigue: The primary muscles used for chewing are the temporalis, masseter, and pterygoid muscles. When the jaw is misaligned or the joint is inflamed, these muscles have to work harder to bring the teeth together. This constant overexertion leads to muscle fatigue and tension. The temporalis muscle, a large, fan-shaped muscle on the side of the head, is a frequent culprit. When it becomes strained, it can cause tension-type headaches that are often felt in the temples.
- Referred Pain: The nerves in the facial region are intricately connected. The trigeminal nerve, one of the largest nerves in the head, provides sensation to the face and controls the chewing muscles. When the TMJ is irritated, it can trigger this nerve, causing pain signals to be sent to other parts of the head. This is known as “referred pain,” where the pain is felt in a location different from its source. This can manifest as a migraine-like headache, sinus pain, or even an earache.
- Bruxism (Teeth Grinding): Many people with TMJ disorders clench or grind their teeth, especially during sleep. This habit places immense force on the jaw joint and surrounding muscles. The constant pressure not only wears down teeth but also leads to morning headaches and facial soreness.
Symptoms to Watch For: Is Your Headache from TMJ?
Because TMJ-related headaches can mimic other types of headaches, it can be difficult to pinpoint the cause. However, there are usually other clues that point to the jaw as the source of the problem. If you experience recurring headaches along with any of the following symptoms, a TMJ disorder could be the underlying issue.
- Pain or tenderness in the jaw, especially upon waking or after chewing.
- A clicking, popping, or grating sound in the jaw joint when opening or closing your mouth.
- Difficulty opening your mouth wide or a feeling that your jaw is “locked” in place.
- Pain in and around your ears that is not related to an infection.
- An uncomfortable or uneven bite, feeling as if your teeth don’t fit together properly.
- Facial pain or a feeling of fatigue in the facial muscles.
- Neck and shoulder pain.
A headache originating from the TMJ is often described as a dull, steady ache that can wrap around the head. It frequently concentrates in the temples, behind the eyes, or at the base of the skull.
Finding Relief: Treatment Options for TMJ Headaches
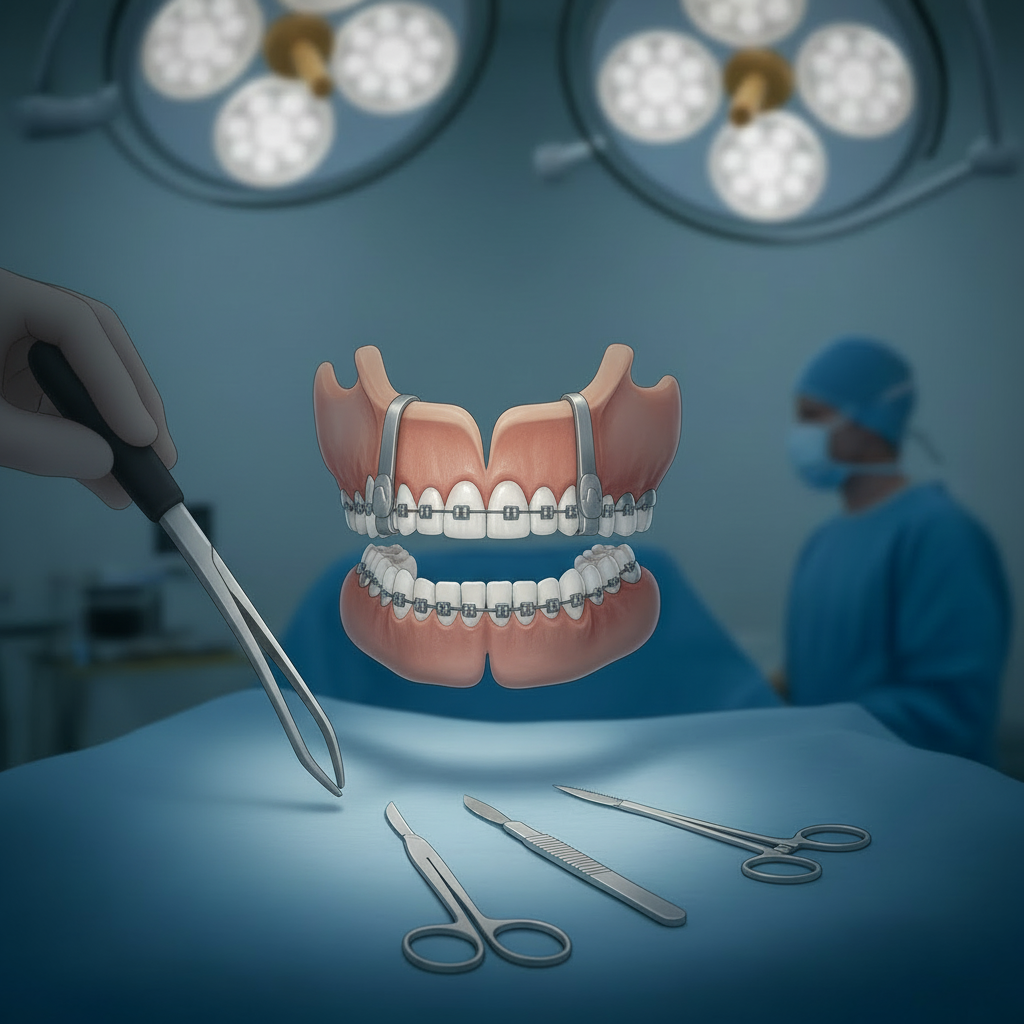
The key to eliminating TMJ-related headaches is to treat the source of the problem: the dysfunctional jaw joint. Treatment is not one-size-fits-all and depends on the severity and cause of the disorder. A specialist will perform a thorough evaluation to create a personalized plan.
Conservative and Non-Surgical Treatments
For many patients, symptoms can be managed effectively with conservative approaches.
- Oral Appliances: A custom-fitted splint or night guard can be worn to prevent teeth grinding and reposition the jaw into a less strenuous position, allowing muscles to relax.
- Physical Therapy: Specific exercises can help stretch and strengthen jaw muscles, improve posture, and increase the range of motion.
- Medications: Anti-inflammatory drugs, muscle relaxants, or in some cases, low-dose antidepressants can help manage pain and reduce muscle tension.
- Lifestyle Modifications: Learning to avoid hard or chewy foods, practicing stress-reduction techniques, and applying moist heat to the jaw can provide significant relief.
Advanced and Surgical Treatments
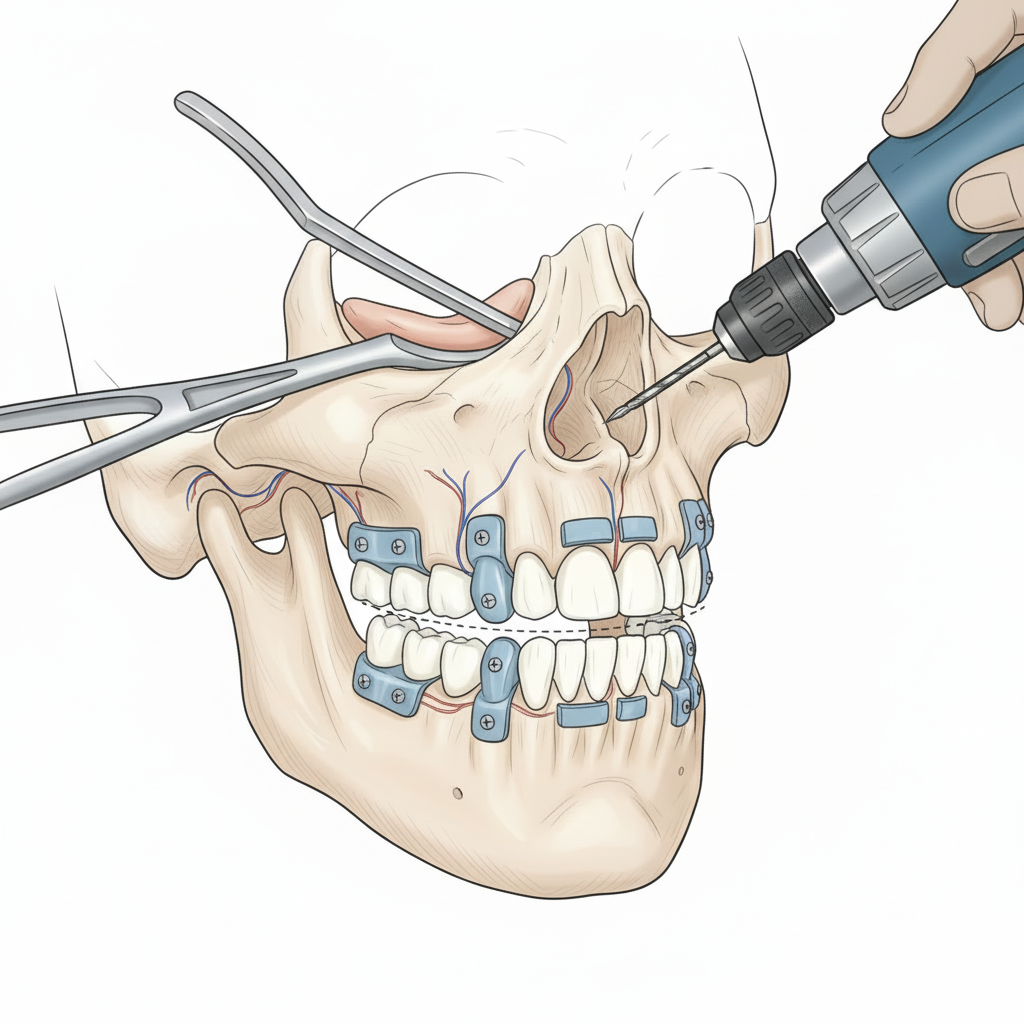
When conservative measures fail to resolve the pain, or if there is significant structural damage to the joint, more advanced intervention may be necessary. Dr. Larry Wolford is a renowned expert in surgical solutions for complex TMJ cases.
- Arthrocentesis: A minimally invasive procedure where the joint is irrigated to flush out inflammatory byproducts.
- TMJ Arthroscopy: A surgeon uses a small camera to view the inside of the joint and perform minor repairs.
- Modified Condylotomy: This procedure addresses internal joint derangement and disc displacement without operating directly on the joint itself.
- Total Joint Replacement: For patients with severe degeneration, a custom-designed artificial joint can be implanted to restore function and permanently eliminate pain.
Case Study: Sarah’s Escape from Chronic Migraines
Sarah, a 38-year-old teacher, had been suffering from debilitating headaches for nearly five years. They were diagnosed as chronic migraines, and she had tried numerous medications with little success. The headaches were often accompanied by a dull ache in her ears and neck stiffness. One day, her dentist noticed significant wear on her molars and asked if she ever experienced jaw popping. Sarah confirmed she did.
Her dentist referred her to Dr. Larry Wolford for a TMJ evaluation. A comprehensive exam and 3D imaging revealed that Sarah had a displaced disc in her right jaw joint and moderate degenerative changes. This dysfunction was causing constant strain on her chewing muscles, which in turn was triggering her chronic headaches.
Dr. Wolford started Sarah on a conservative treatment plan, beginning with a custom-made oral splint to decompress her jaw joint and relax her muscles. Within a few weeks of wearing the splint at night, Sarah noticed a remarkable difference. Her morning headaches became less frequent and less intense. After several months of splint therapy combined with physical therapy, her headaches disappeared completely. Sarah’s case shows how accurately diagnosing a TMJ disorder as the source of head pain can lead to effective and often non-invasive treatment.
Don’t Let Headaches Control Your Life
Living with chronic headaches is draining, but you don’t have to accept it as your normal. If you’ve tried other treatments without success and suspect your jaw might be involved, it is time to seek a specialist’s opinion. A proper diagnosis can set you on the right path to becoming pain-free.
To learn more about the link between jaw function and head pain, you can explore more about The Connection Between TMJ Disorders and Headaches. A consultation with an expert can provide the clarity and solutions you need to improve your quality of life.
Helpful Resources
- The TMJ Association: An organization providing support and science-based information to patients.
- American Migraine Foundation: Offers resources on different types of headaches and their causes.