Welcome to the world of precision and expertise in maxillofacial surgery! From jaw correction to TMJ surgery, the realm of oral and maxillofacial surgery is a fascinating blend of artistry and science. In this blog post, we delve into the intricate principles guiding maxillofacial procedures, the advanced diagnostic techniques employed for jaw correction and TMJ issues, as well as the transformative outcomes that skilled surgeons can achieve. Let’s embark on a journey through the intricacies of maxillofacial surgery together!
Definition of Maxillofacial Surgery
Maxillofacial surgery is a specialized branch of medicine that focuses on treating conditions affecting the face, jaw, and mouth. It encompasses a wide range of procedures aimed at correcting deformities, injuries, or diseases in the oral and facial regions. Surgeons in this field undergo extensive training to master the intricacies of facial anatomy and surgical techniques specific to this area.
The scope of maxillofacial surgery extends beyond cosmetic enhancements to include trauma management, oncology treatments, orthognathic surgeries for jaw correction, and TMJ surgeries for addressing temporomandibular joint disorders. By combining surgical expertise with an understanding of dental and craniofacial structures, maxillofacial surgeons play a crucial role in restoring function and aesthetics to their patients’ faces.
With advancements in technology and interdisciplinary collaboration with other healthcare professionals like orthodontists and ENT specialists, maxillofacial surgeons can provide comprehensive care tailored to each patient’s unique needs. This dynamic field continues to evolve as new techniques emerge, offering hope and transformation to those seeking treatment for complex oral and facial conditions.
Scope of Maxillofacial Surgery Jaw correction TMJ surgery Trauma management Oncology Orthognathic surgery
Maxillofacial surgery encompasses a wide range of surgical procedures aimed at correcting jaw abnormalities, treating TMJ disorders, managing trauma injuries, addressing oncological conditions, and performing orthognathic surgeries.
Jaw correction procedures focus on realigning the jaws to improve function and aesthetics. They can involve osteotomies or genioplasty to enhance facial harmony.
TMJ surgery targets issues affecting the temporomandibular joint, alleviating pain and restoring proper function through techniques like joint reconstruction or disc repositioning.
Trauma management in maxillofacial surgery involves repairing fractures and soft tissue injuries resulting from accidents or other traumatic events.
Oncology within this specialty deals with diagnosing and surgically treating tumors affecting the head and neck region.
Orthognathic surgery aims to correct skeletal irregularities of the face and jaws for functional improvement and enhanced facial aesthetics.
Principles of Maxillofacial Surgery Anatomical Knowledge Bone structure Muscles Nerves
Understanding the principles of maxillofacial surgery requires a deep knowledge of anatomy. The bone structure of the face is complex, with various bones forming the foundation for facial aesthetics and function. Surgeons must have a detailed understanding of how these bones interact and contribute to overall facial harmony.
Muscles play a crucial role in jaw movement and facial expressions. Surgeons need to be well-versed in muscle anatomy to ensure proper function post-surgery. Nerves are delicate structures that control sensation and movement in the face. Protecting these nerves during surgery is paramount to avoid complications such as numbness or paralysis.
Anatomical knowledge serves as the cornerstone for successful maxillofacial procedures. It guides surgeons in their approach, ensuring precision and optimal outcomes for patients undergoing jaw correction or TMJ surgery.
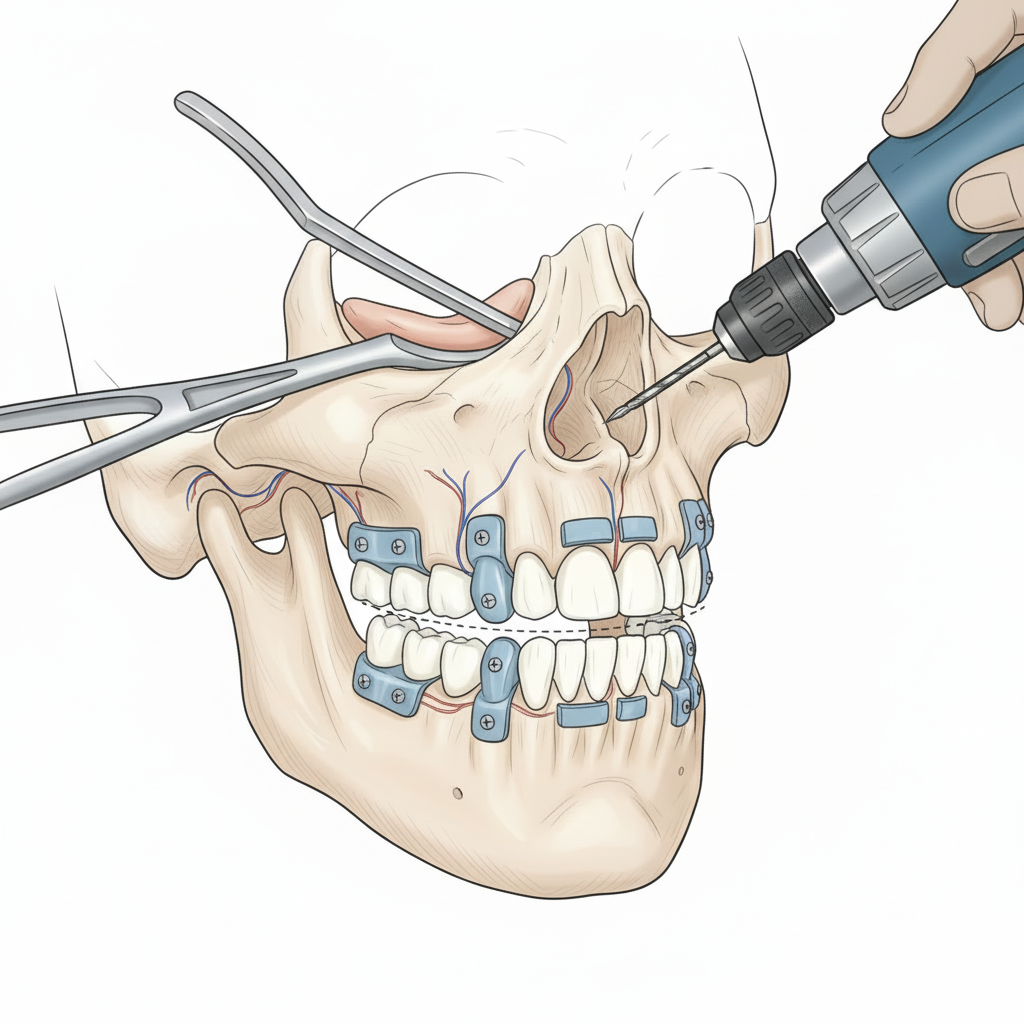
Surgical Techniques Aseptic techniques Incision and closure techniques Bone manipulation
When it comes to maxillofacial surgery, surgical techniques play a crucial role in ensuring successful outcomes. Aseptic techniques are meticulously followed to prevent infections and promote healing post-surgery.
Incision and closure techniques are skillfully performed to minimize scarring and optimize the aesthetic result for patients undergoing jaw correction or TMJ surgery. Surgeons pay close attention to detail when making incisions and suturing wounds.
Bone manipulation is a precise art in maxillofacial surgery, where surgeons reshape or reposition the jaw bone to improve function and aesthetics. By utilizing advanced tools and techniques, bone manipulation is carried out with utmost care and precision for optimal results.
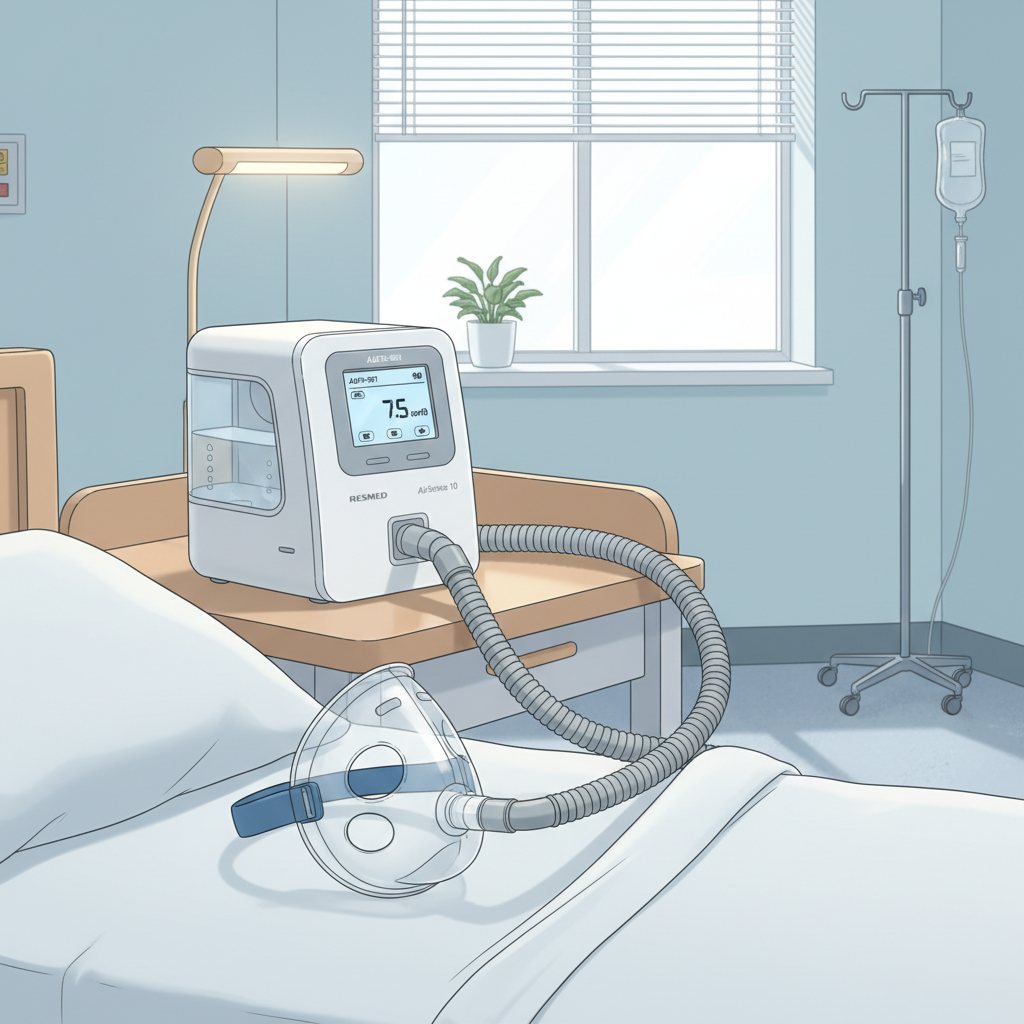
Patient Safety Preoperative assessment Intraoperative monitoring Postoperative care
Patient safety is a top priority in maxillofacial surgery, starting with thorough preoperative assessments. These evaluations help ensure the patient is medically fit for surgery and that potential risks are identified and managed appropriately.
During the intraoperative phase, continuous monitoring of vital signs and anesthesia levels ensures a safe surgical experience. Close attention to detail by the surgical team helps maintain patient stability throughout the procedure.
Postoperatively, diligent care is provided to optimize recovery and minimize complications. Pain management strategies tailored to individual needs, along with clear post-op instructions, play a crucial role in promoting healing and comfort for patients.
By focusing on comprehensive preoperative assessments, meticulous intraoperative monitoring, and attentive postoperative care, maxillofacial surgeons uphold high standards of patient safety at every stage of treatment.
Interdisciplinary Approach Coordination with orthodontists, ENT specialists, and other healthcare providers
When it comes to Maxillofacial surgery, collaboration is key. The interdisciplinary approach involves a seamless coordination between various healthcare providers to ensure comprehensive patient care.
Orthodontists play a crucial role in aligning teeth and jaws before and after surgical procedures. Their expertise in dental alignment complements the work of maxillofacial surgeons.
ENT specialists bring their knowledge of ear, nose, and throat anatomy to address any related issues that may impact the success of jaw correction or TMJ surgeries.
This harmonious teamwork ensures that patients receive holistic care tailored to their specific needs. By combining the skills and insights of different specialists, patients can benefit from a well-rounded treatment plan that addresses all aspects of their condition.
The collaboration fosters innovation, allowing for creative solutions and personalized approaches to complex cases. Together, these healthcare professionals strive towards optimal outcomes for every patient who walks through their doors.
Use of Technology Imaging techniques (CT, MRI, 3D imaging) Computer-aided design and manufacturing (CAD/CAM)
In the field of maxillofacial surgery, technology plays a crucial role in enhancing precision and outcomes. Imaging techniques like CT scans, MRI, and 3D imaging offer detailed views of the jaw and surrounding structures, aiding in accurate diagnosis and treatment planning.
Additionally, computer-aided design and manufacturing (CAD/CAM) have revolutionized surgical procedures by allowing for customized implants and prosthetics tailored to each patient’s unique anatomy. This technology ensures a perfect fit and optimal functionality post-surgery.
By integrating these advanced technological tools into practice, maxillofacial surgeons can deliver personalized care with improved results. The use of cutting-edge imaging and CAD/CAM systems continues to push the boundaries of what is possible in oral and maxillofacial surgery.

Diagnosis of Maxillofacial Conditions for Jaw Correction Patient History and Examination Medical and dental history Symptom assessment (pain, dysfunction)
When it comes to diagnosing maxillofacial conditions for jaw correction, thorough patient history and examination are key. Medical and dental histories provide valuable insights into the patient’s overall health and any pre-existing conditions that may impact treatment.
Symptom assessment plays a crucial role in understanding the patient’s experience, especially regarding pain levels and functional limitations. By listening attentively to the patient’s description of their symptoms, healthcare providers can better tailor their diagnostic approach.
Examining the medical records alongside conducting a comprehensive physical evaluation helps paint a clearer picture of the underlying issues causing jaw misalignment or dysfunction. This holistic approach ensures that all aspects of the patient’s health are considered before proceeding with further diagnostic tests or treatment options.
Through detailed medical history taking, dental examinations, and symptom assessments, healthcare professionals can begin to unravel the complexities of maxillofacial conditions requiring jaw correction interventions.
Clinical Examination Extraoral and intraoral examination Palpation of the TMJ and jaw muscles
When it comes to diagnosing issues related to the jaw and temporomandibular joint (TMJ), clinical examinations play a crucial role. During an extraoral examination, the maxillofacial surgeon will observe the patient’s facial symmetry, jaw movements, and alignment.
Intraoral examinations involve assessing the condition of the oral cavity, teeth alignment, and bite relationship. Palpation of the TMJ area allows for detecting any tenderness or abnormalities in the joint itself. By examining how the jaw muscles function during movement and at rest, surgeons can identify potential issues affecting jaw mobility.
The detailed evaluation of these areas helps in determining treatment options tailored to each patient’s specific needs. Through thorough palpation techniques and observations, maxillofacial surgeons can gather valuable information essential for accurate diagnosis and effective treatment planning.
Imaging Studies X-rays (panoramic, cephalometric) CT scans MRI (for soft tissue evaluation)
When it comes to diagnosing maxillofacial conditions for jaw correction or TMJ surgery, imaging studies play a crucial role in providing detailed insights into the patient’s anatomy. X-rays, including panoramic and cephalometric views, offer valuable information about the teeth alignment and bone structure of the jaw.
CT scans are commonly used in maxillofacial surgery to provide detailed 3D images of the bones and surrounding tissues. This advanced imaging technique allows surgeons to visualize complex anatomical structures with precision.
MRI is particularly beneficial for evaluating soft tissues like muscles, ligaments, and discs within the temporomandibular joint. By using magnetic resonance imaging, healthcare providers can assess any abnormalities or damage in these delicate structures that may be causing pain or dysfunction for the patient.
Integrating various imaging modalities such as X-rays, CT scans, and MRI ensures a comprehensive approach to diagnosing maxillofacial conditions accurately and planning optimal treatment strategies for patients requiring jaw correction or TMJ surgery.
Functional Assessments Occlusal analysis Jaw movement analysis
Functional assessments play a crucial role in determining the effectiveness of jaw correction procedures. Occlusal analysis involves evaluating how the teeth fit together when the jaw is closed, helping to identify any misalignments that may contribute to issues like TMJ dysfunction. By assessing occlusion, maxillofacial surgeons can better plan for corrective measures during surgery.
Jaw movement analysis focuses on studying the range and symmetry of movements in the temporomandibular joint (TMJ). This assessment aids in understanding any limitations or abnormalities present in jaw mobility, which can impact a patient’s ability to chew, speak, and even breathe properly. Understanding these movement patterns is essential for developing personalized treatment plans tailored to each individual’s needs.
Through comprehensive functional assessments like occlusal analysis and jaw movement analysis, maxillofacial surgeons gain valuable insights into the underlying causes of patients’ dental and skeletal irregularities. These evaluations help guide surgical interventions towards achieving optimal outcomes and restoring proper function to the jaws and facial structures.
Orthodontic Evaluation Dental alignment Bite relationship
When it comes to evaluating the alignment of your teeth and their relationship when you bite down, orthodontists play a crucial role in ensuring everything is in harmony.
Through a thorough examination, they assess how your upper and lower teeth fit together – known as your bite relationship. This evaluation helps determine if there are any issues like overbite, underbite, or crossbite that may require correction.
Orthodontic evaluations also involve analyzing the positioning of individual teeth to see if there are overcrowding, spacing issues, or misalignments that could impact your overall oral health and function.
By carefully examining these factors, orthodontists can develop personalized treatment plans using braces, aligners, or other appliances to help straighten your teeth and improve your bite for optimal dental health.
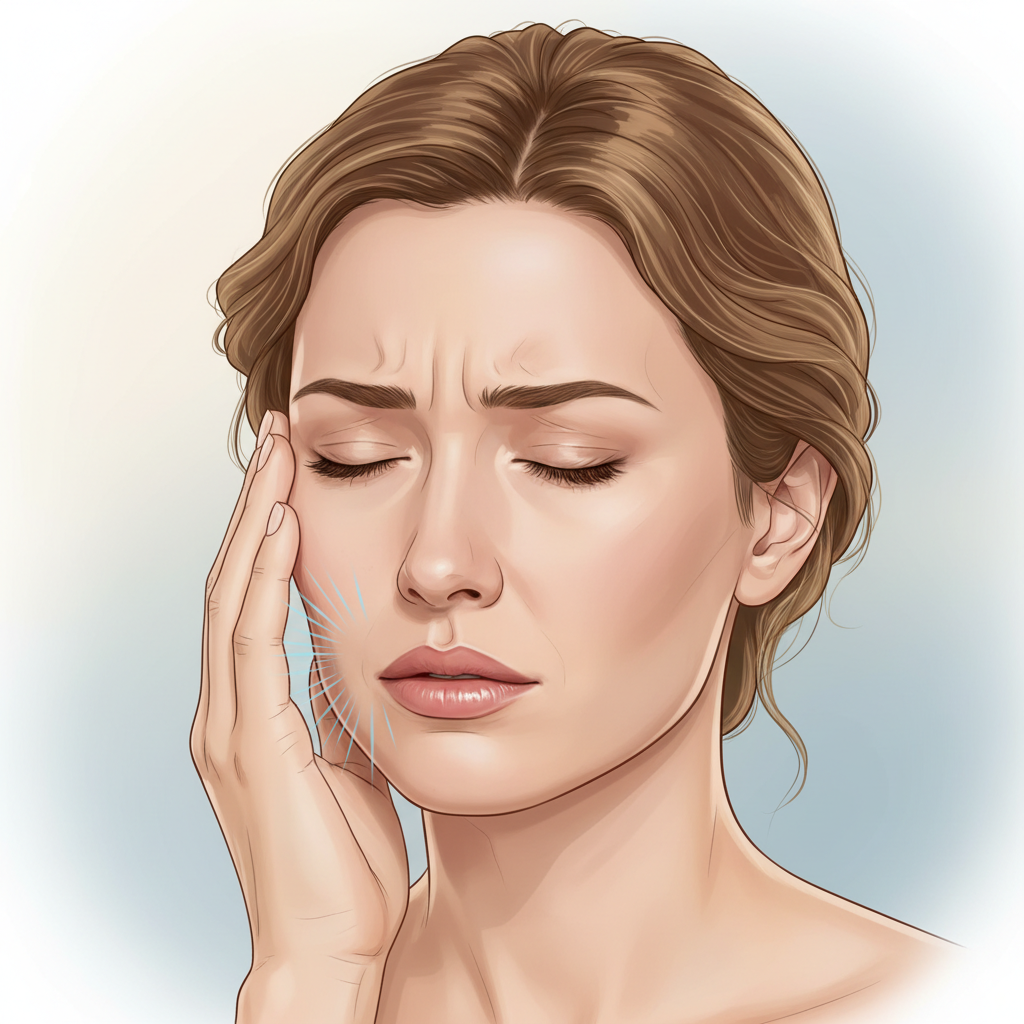
Diagnosis of Maxillofacial Conditions for TMJ Surgery Patient History and Examination Detailed TMJ history (clicking, popping, pain) Previous treatments and outcomes
When it comes to diagnosing maxillofacial conditions for TMJ surgery, a thorough patient history and examination are crucial. Detailed questioning about TMJ symptoms like clicking, popping, and pain helps in understanding the extent of the issue. Previous treatments and their outcomes provide valuable insights into the patient’s journey with TMJ disorders.
The detailed TMJ history allows the healthcare provider to understand the progression of symptoms and any triggering factors that may be present. Examining how previous treatments have impacted the condition guides in determining further steps for effective management.
By delving deep into the patient’s experience with TMJ issues, healthcare providers can tailor treatment plans that address specific concerns and improve quality of life. Understanding past interventions helps in crafting personalized approaches to alleviate discomfort and enhance jaw function.
Clinical Examination Palpation of the TMJ Range of motion assessment Joint sounds evaluation
During a clinical examination for temporomandibular joint (TMJ) issues, palpation is key. By gently feeling the jaw joint and surrounding muscles, healthcare providers can assess for tenderness, swelling, or abnormalities. This hands-on approach helps in identifying potential areas of concern that may be causing TMJ symptoms.
Additionally, assessing the range of motion of the jaw is crucial. By observing how far a patient can comfortably open and close their mouth, clinicians can gather important information about any restrictions or limitations in movement. Any pain or clicking sounds during this assessment could indicate underlying TMJ problems.
Furthermore, evaluating joint sounds during jaw movements provides valuable insights into the health of the TMJ. Clicking, popping, or grinding noises may suggest issues with the disc within the joint or abnormal bone alignment. These auditory clues play a significant role in diagnosing TMJ disorders accurately.
In summary…
Imaging Studies MRI (for disc position and joint structures) Arthrography (for internal joint structures) CT scans (for bony structures)
When it comes to diagnosing maxillofacial conditions for jaw correction and TMJ surgery, imaging studies play a crucial role in providing detailed insights that help guide treatment plans. Magnetic Resonance Imaging (MRI) is commonly used to assess the position of the disc and evaluate the joint structures within the temporomandibular joint.
Arthrography is another imaging technique utilized to visualize internal joint structures with precision, aiding in identifying specific issues that may not be visible through other methods. This procedure involves injecting contrast dye into the joint space before taking X-rays or CT scans, enhancing visibility and accuracy in diagnosis.
CT scans are valuable for capturing detailed images of bony structures around the jaw and skull region. By providing clear 3D visuals, CT scans enable healthcare providers to analyze bone architecture and detect any abnormalities or injuries that may require surgical intervention.

Functional Assessments Jaw tracking and movement analysis Bite force measurement
When it comes to diagnosing jaw-related issues, functional assessments play a crucial role in understanding the dynamics of how the jaw functions.
Jaw tracking and movement analysis involve evaluating the range of motion, alignment, and coordination during various activities such as opening, closing, and lateral movements of the jaw.
Bite force measurement helps assess the strength exerted by the jaws when biting down or chewing. This measurement aids in identifying any imbalances or abnormalities in muscle function that may be contributing to jaw pain or dysfunction.
By conducting these assessments, healthcare providers can gather valuable information about an individual’s jaw functionality to determine appropriate treatment plans tailored to address specific concerns related to jaw movement and bite force.
Pain Assessment Pain scales and questionnaires Trigger point examination
When it comes to assessing pain in maxillofacial conditions, various tools and techniques are utilized. Pain scales and questionnaires help patients articulate their discomfort levels, aiding healthcare providers in understanding the severity of their symptoms. These standardized assessments provide valuable insights into the patient’s experience, guiding tailored treatment plans.
Additionally, trigger point examination is crucial in identifying specific areas of tenderness or muscle tightness that may be contributing to jaw or TMJ pain. By pinpointing these trigger points, clinicians can target interventions more effectively for symptom relief. This hands-on assessment technique is an essential component of a comprehensive evaluation for individuals seeking maxillofacial care.
Understanding and addressing pain is fundamental in optimizing patient outcomes and enhancing quality of life. By utilizing these assessment methods, healthcare professionals can tailor treatment strategies to alleviate discomfort and improve overall well-being for those undergoing maxillofacial surgery procedures.
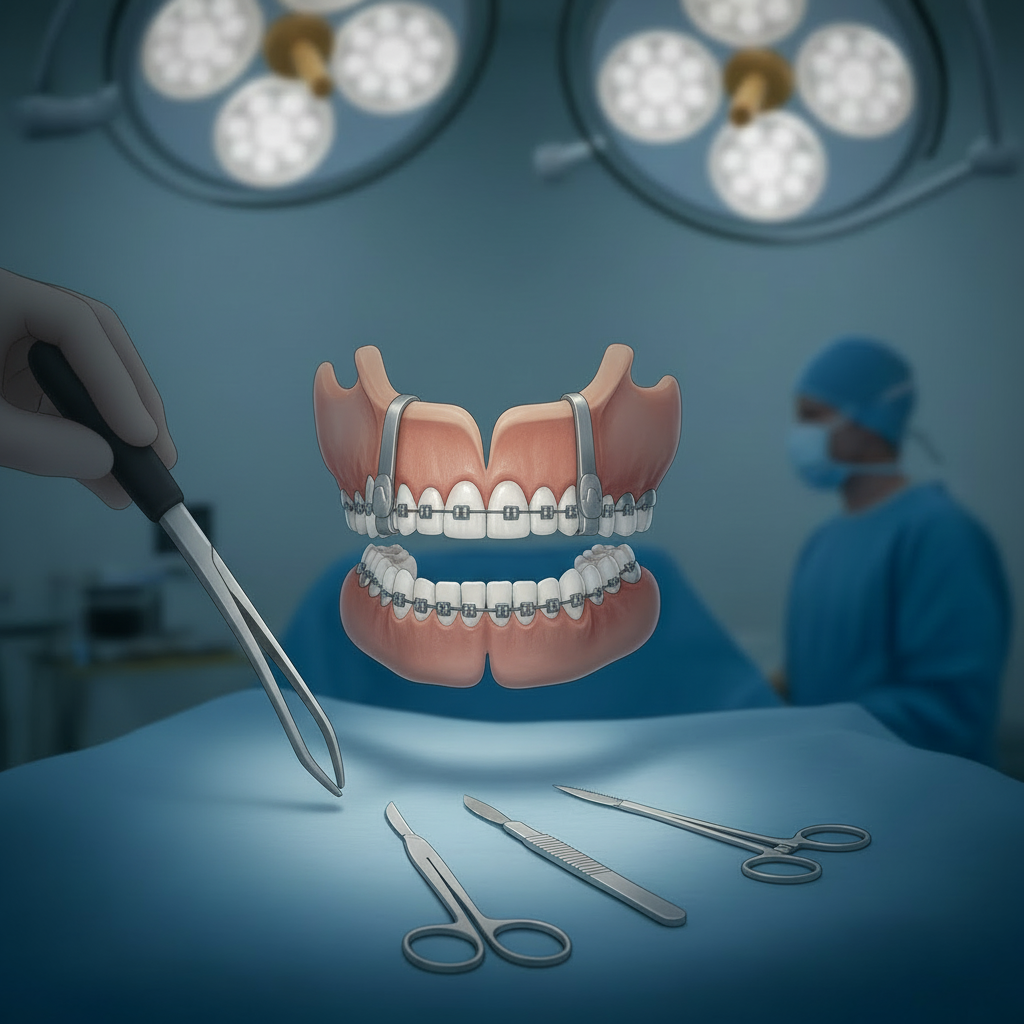
Treatment Planning for Jaw Correction Interdisciplinary Planning Collaboration with orthodontists Comprehensive treatment plan
When it comes to planning jaw correction treatments, collaboration is key. Maxillofacial surgeons work closely with orthodontists to create comprehensive treatment plans that address both functional and aesthetic concerns.
Orthodontists play a crucial role in aligning teeth before and after jaw surgery, ensuring optimal results. Their expertise complements the surgical aspect of the treatment, leading to successful outcomes for patients seeking jaw correction.
By integrating orthodontic care into the overall plan, patients benefit from a holistic approach that considers all aspects of their oral health. This interdisciplinary collaboration maximizes the effectiveness of jaw correction procedures and enhances long-term stability.
Together, maxillofacial surgeons and orthodontists combine their skills to tailor individualized treatment plans based on each patient’s unique needs. This teamwork results in transformative changes that not only improve facial harmony but also enhance function and quality of life.
In essence, the coordination between these two specialties symbolizes a harmonious blend of artistry and science aimed at achieving optimal outcomes for those undergoing jaw correction procedures.
Surgical Options Orthognathic surgery (mandibular and maxillary osteotomies) Genioplasty (chin surgery)
Maxillofacial surgeons offer various surgical options to correct jaw abnormalities and enhance facial harmony. Orthognathic surgery involves mandibular and maxillary osteotomies, which are precise bone cuts to reposition the jaws for improved function and aesthetics.
On the other hand, genioplasty focuses on enhancing the chin’s shape and position. This procedure can be standalone or combined with other surgeries to achieve balanced facial proportions.
Orthognathic surgery requires careful planning and coordination between the surgeon, orthodontist, and other specialists. It aims to address functional issues like bite alignment as well as improve facial symmetry.
Genioplasty is tailored to each patient’s unique needs, offering a personalized approach to chin augmentation or reduction. By utilizing advanced surgical techniques, maxillofacial surgeons can help patients achieve their desired facial profile with natural-looking results.
Preoperative Preparations
Preparing for maxillofacial surgery involves various critical steps to ensure a smooth and successful procedure. One essential aspect of preoperative preparations is orthodontic treatment before the surgical intervention. This may involve aligning the teeth and jaws to improve the overall function and aesthetics.
Apart from orthodontic considerations, nutritional preparation plays a vital role in optimizing healing post-surgery. A well-balanced diet rich in nutrients can aid in tissue repair and recovery, promoting better outcomes.
Furthermore, psychological preparation is key to addressing any anxieties or concerns patients may have before undergoing maxillofacial surgery. Counseling or therapy sessions can help individuals feel more mentally prepared for the upcoming procedure.
By focusing on these aspects of preoperative care, patients can enhance their overall experience and set themselves up for a successful outcome following maxillofacial surgery.
Postoperative Care Pain management Physical therapy Follow-up appointments
Once the maxillofacial surgery is successfully completed, postoperative care becomes crucial for a smooth recovery. Pain management strategies are tailored to each patient’s needs, ensuring comfort during the healing process.
Physical therapy plays a key role in regaining jaw function and strengthening muscles post-surgery. These exercises aid in restoring mobility and reducing stiffness, promoting optimal recovery outcomes.
Follow-up appointments with your maxillofacial surgeon are scheduled to monitor progress, address any concerns, and track healing. These visits allow for timely adjustments to the treatment plan if needed, ensuring the best possible results from your surgery.
Diligent adherence to postoperative care instructions and attending follow-up appointments is essential for a successful recovery journey after maxillofacial surgery.
Treatment Planning for TMJ Surgery
When it comes to planning for TMJ surgery, conservative treatments play a crucial role in alleviating symptoms and improving jaw function. Medications such as NSAIDs and muscle relaxants are commonly used to manage pain and reduce inflammation in the temporomandibular joint.
Physical therapy is another key component of treatment planning for TMJ surgery. It focuses on strengthening the jaw muscles, improving jaw mobility, and promoting proper alignment of the joint. Through targeted exercises and interventions, physical therapists can help patients regain optimal function in their jaws.
In some cases, occlusal splints may be recommended as part of conservative treatment for TMJ disorders. These custom-made oral appliances help stabilize the bite, reduce clenching or grinding habits, and provide cushioning for the joint during movement.
By combining these conservative approaches in the treatment plan for TMJ surgery, healthcare providers aim to optimize outcomes and enhance patient comfort before considering more invasive procedures. Each step is tailored to address individual needs and promote overall well-being throughout the healing process.
Minimally Invasive Procedures Arthrocentesis Arthroscopy
When it comes to addressing temporomandibular joint (TMJ) issues, minimally invasive procedures like arthrocentesis and arthroscopy play a crucial role in providing effective treatment options.
Arthrocentesis involves the flushing of the TMJ with sterile fluid to remove debris and reduce inflammation, helping improve jaw function and alleviate pain. This minimally invasive technique can often be performed on an outpatient basis, offering patients a quicker recovery time compared to traditional open surgeries.
On the other hand, arthroscopy utilizes small incisions and a tiny camera to visualize the inside of the joint, allowing surgeons to diagnose and treat TMJ conditions with precision. By targeting specific areas within the joint, arthroscopy can help address issues such as disc displacement or arthritis while minimizing tissue damage.
Both arthrocentesis and arthroscopy represent innovative approaches in maxillofacial surgery that prioritize patient comfort and successful outcomes. These less invasive techniques continue to evolve, offering promising solutions for individuals seeking relief from TMJ disorders.
Open Surgical Procedures
When it comes to addressing more complex TMJ issues, open surgical procedures like joint reconstruction or disc repositioning may be necessary. These interventions aim to restore proper function and alleviate pain associated with the temporomandibular joint.
After undergoing such surgeries, postoperative care becomes crucial for successful recovery. This includes effective pain management strategies tailored to each patient’s needs and comfort level.
Physical therapy often plays a key role in the rehabilitation process following these surgical interventions. It helps improve jaw mobility, strengthen muscles, and promote overall healing of the affected area.
Long-term monitoring is essential after undergoing open surgical procedures for TMJ conditions. Regular follow-up appointments allow healthcare providers to assess progress, address any concerns that may arise, and ensure optimal outcomes in the long run.
Case Studies and Outcomes Jaw Correction
Let’s delve into some real-life success stories in jaw correction through orthognathic surgeries.
One case study involved a patient with severe malocclusion and facial asymmetry. After undergoing orthognathic surgery to correct the misalignment, the patient achieved not only functional improvement but also a significant enhancement in facial aesthetics.
In another instance, a young individual struggling with difficulty chewing and speaking due to jaw misalignment opted for orthognathic surgery. Post-surgery, they experienced a remarkable transformation in their quality of life, regaining proper jaw function and confidence in their appearance.
Patient testimonials often highlight the life-changing impact of successful orthognathic surgeries. From improved bite alignment to enhanced facial harmony, these stories showcase the profound benefits that can result from precision jaw correction procedures.
These real cases underscore the transformative power of maxillofacial surgery in restoring both function and aesthetics for individuals seeking comprehensive treatment for their jaw concerns.

TMJ Surgery Case Studies
TMJ surgery can greatly improve the quality of life for individuals suffering from temporomandibular joint disorders. Let’s explore some real-life case studies showcasing successful TMJ surgeries and hear directly from patients who underwent these procedures.
Case Study 1: Sarah, a 35-year-old teacher, had been experiencing severe jaw pain and limited mouth opening due to TMJ dysfunction. After undergoing arthroscopy to address internal joint derangement, she now enjoys pain-free chewing and speaking without discomfort.
Case Study 2: John, a 42-year-old accountant, struggled with chronic jaw clicking and muscle stiffness. Following a joint reconstruction surgery to repair damaged tissues, he experienced significant relief and regained normal jaw function.
Patient Testimonial: “I never imagined life without constant jaw pain until I had TMJ surgery. It’s truly been life-changing for me,” says Lily, a 28-year-old artist who found relief after disc repositioning surgery.
These success stories highlight the positive impact of TMJ surgeries on restoring oral health and enhancing overall well-being.
Summary of Key Points Future Directions in Maxillofacial Surgery Advances in technology Research and innovation
As we look towards the future of maxillofacial surgery, exciting advancements are on the horizon. Technology continues to evolve, providing surgeons with innovative tools and techniques to improve patient outcomes. Research in this field is constantly pushing boundaries, leading to new discoveries and treatment options.
Innovation plays a crucial role in shaping the future of maxillofacial surgery, offering patients more personalized and effective care. From 3D imaging for precise surgical planning to computer-aided design for custom implants, the possibilities are endless. Collaboration between professionals across various disciplines will further enhance patient care and treatment success rates.
With a focus on continuous improvement and excellence, maxillofacial surgeons are dedicated to staying at the forefront of medical innovation. By embracing cutting-edge technologies and advancing research efforts, the future of maxillofacial surgery looks promising – paving the way for enhanced patient experiences and superior clinical outcomes.
References Key Textbooks and Articles Professional Guidelines and Standards Relevant Case Studies and Clinical Trials
Maxillofacial surgery is a dynamic field that combines surgical expertise with a deep understanding of facial anatomy and function. From jaw correction to TMJ surgery, maxillofacial surgeons play a vital role in improving patients’ quality of life.
By adhering to the principles of maxillofacial surgery, utilizing advanced technologies for diagnosis and treatment planning, and collaborating with multidisciplinary healthcare teams, these specialists can achieve remarkable outcomes for their patients.
As the field continues to evolve with technological advancements and innovative research, the future of maxillofacial surgery holds promising possibilities for further enhancing patient care and outcomes.
For those interested in delving deeper into this fascinating specialty, exploring key textbooks, articles, professional guidelines, relevant case studies, and clinical trials will provide valuable insights into the latest trends and best practices in maxillofacial surgery.