The prospect of oral surgery can be intimidating to many patients, but knowing what to expect throughout the treatment process can help to ease any fears or anxieties that arise. For example, if you realize that your initial consultation is unlikely to involve much more than a visual examination and x-rays, then you can approach that appointment with a more positive attitude.
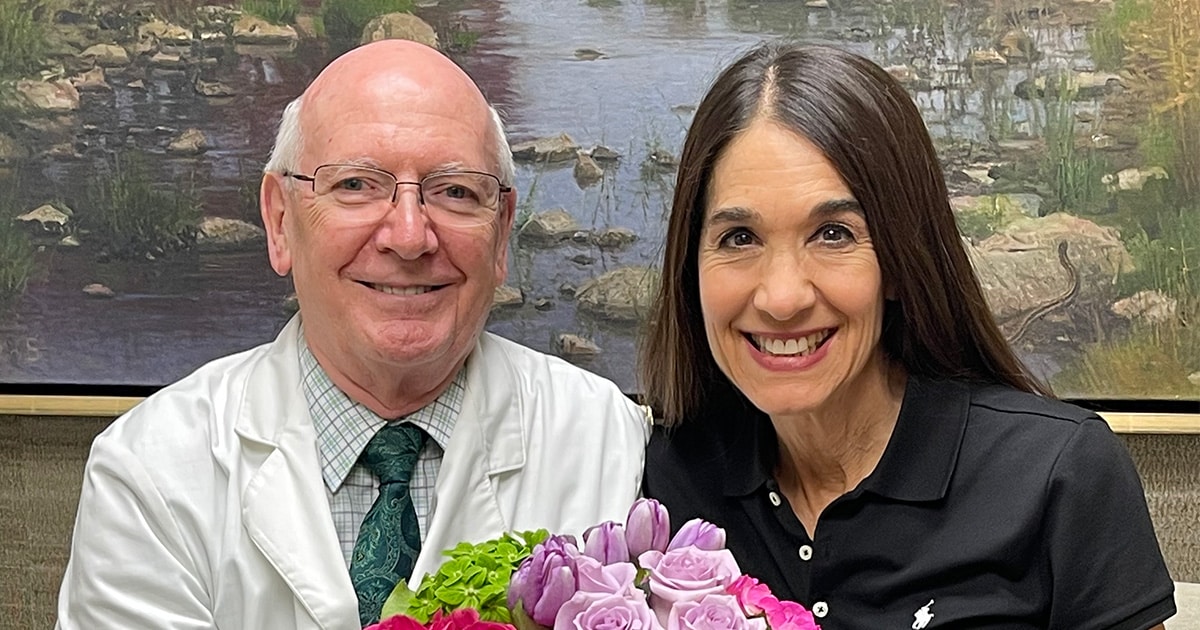
The best oral surgeon will also take advantage of that first appointment to begin to establish a productive working relationship with the patient, and that can also be important in achieving the desired treatment outcomes.
Patients may see an oral surgeon for several reasons, including corrective jaw surgery to repair a congenital defect or damage done by trauma, wisdom tooth extraction, or to have suspicious tissue removed and biopsied. Oral surgeons in Dallas, TX, can provide interventions for conditions as varied as sleep apnea and temporomandibular joint (TMJ) disorders that can have a negative effect on your health and well-being.
Your Oral Surgery Initial Consultation is Important
Regardless of the specific nature of your treatment, your oral surgeon will begin treatment planning at the initial consultation by collecting a significant amount of data that will be needed to inform your treatment plan. The surgeon will visually inspect your jaws and take x-rays.
The surgeon may also discuss pre-operative and post-operative instructions with you the first time that you come to the office. It’s important to be sure that you understand these directions to reduce your chances of complications with the surgery and increase the likelihood that you’ll have an uneventful recovery.
The initial consultation also gives you the opportunity to discuss any concerns that you may have and get answers to your questions. Feel free to ask the surgeon anything. No question is too minor or silly.