Are you experiencing discomfort or limited movement in your jaw? TMJ replacement surgery might be the solution you’ve been searching for. In this comprehensive guide, we’ll delve into what TMJ replacement surgery entails, when it’s necessary, and what to expect during the procedure. Join us on a journey to discover how this innovative surgery could transform your quality of life!
TMJ replacement surgery, or total temporomandibular joint replacement is a relatively new surgical procedure that involves replacing the joints between the lower jaw and the base of the skull with custom-made prosthetic joints.
Dr. Larry Wolford Is One of the Top TMJ Surgery Specialists in the U.S.
TMJ replacement surgery, also known as total temporomandibular joint replacement, is a groundbreaking procedure designed to address issues in the joints connecting your lower jaw to the base of your skull. This innovative surgery involves the customization and implantation of prosthetic joints tailored specifically for each patient’s unique needs.
Dr. Larry Wolford stands out as a top specialist in the UK who offers this advanced surgical option to patients dealing with severe TMJ disorders or complications. With his expertise and experience, he brings a high level of precision and care to every TMJ replacement surgery he performs.
By utilizing custom-made prosthetic joints, Dr. Larry Wolford aims to restore proper function and alleviate pain for individuals struggling with debilitating jaw conditions. Through this specialized approach, patients can regain mobility and improve their overall quality of life under his expert guidance.
How Common Are Jaw Problems?
Jaw problems are relatively common; these range from mild jaw clicking to more serious jaw locking and joint degeneration or traumatic damage. The range of problems can be as extensive as with any joint in the body, and while hip and knee replacement surgery has been perfected over many years, being confident of success with jaw joint procedures has only been possible in the last 10-15 years.
Jaw problems can be more common than you might think. From mild jaw clicking to severe joint degeneration, issues with the temporomandibular joint (TMJ) can vary in severity. Unlike hip and knee replacements which have been refined over decades, TMJ procedures have only recently seen advancements in success rates.
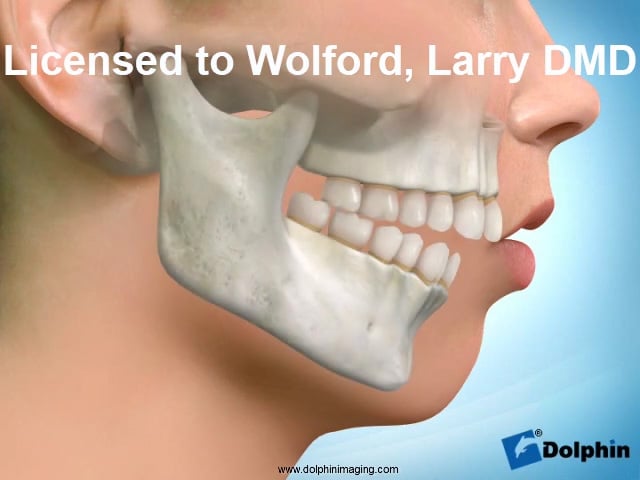
The complexity of the jaw joint mirrors that of any other in the body, presenting a range of challenges for those affected. While some may experience occasional discomfort or clicking, others face debilitating pain and limited mobility due to conditions like osteoarthritis or traumatic injuries.
Thanks to advancements in medical technology and expertise, patients now have access to specialized treatments like TMJ replacement surgery provided by skilled professionals such as Dr. Larry Wolford. This allows individuals suffering from severe jaw issues to regain function and alleviate their symptoms effectively within recent years.

Do I Need TMJ Jaw Replacement Surgery?
TMJ treatment (jaw replacement surgery) is usually required in patients who have:
- Jaw damage through osteoarthritis
- Damage due to an accident
- Had part of the jaw bone removed due to a cancerous tumor, bone infection, rheumatoid or psoriatic arthritis.
Jaw Replacement Surgery Is Not Required for All Kinds of Jaw Problems
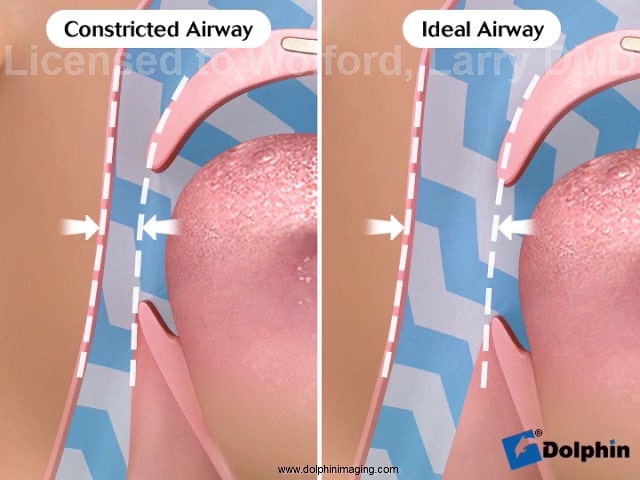
Some problems can be solved by looking inside the joint with a scope and washing the joint out. Dr. Larry Wolford uses the very latest tiny scopes that are just over 1mm in diameter and can be used to examine the inside of the joint directly.
Injections are also offered to relieve inflammation and TMJ pain that may provide enough relief for the patient. Surgery remains an option if the symptoms return in the future. Patients who have a seriously damaged TMJ experience limited movement and pain that can be debilitating.
With severe TMJ disorder the patient usually can’t talk or swallow their own saliva without severe pain. A TMJ replacement can be a huge benefit to these patients.
TMJ replacement surgery, or total temporomandibular joint replacement, is a specialized procedure that becomes necessary in cases where patients experience severe jaw damage. This can result from conditions like osteoarthritis, traumatic accidents, or even the removal of part of the jaw bone due to serious health issues such as cancerous tumors or infections.
In some instances, less invasive treatments like scopes and injections may provide temporary relief for TMJ pain and inflammation. However, for individuals facing significant limitations in movement and unbearable pain due to advanced TMJ disorders, surgical intervention with a jaw replacement might be the most effective solution.
Dr. Larry Wolford utilizes cutting-edge technology like tiny scopes to directly examine the joint’s interior and offers tailored treatment plans based on individual needs. For those struggling with debilitating symptoms that impact basic functions like speaking or swallowing without immense discomfort, undergoing a TMJ replacement surgery could potentially offer substantial improvements in their quality of life.
What Does TMJ Replacement Surgery Consist Of?
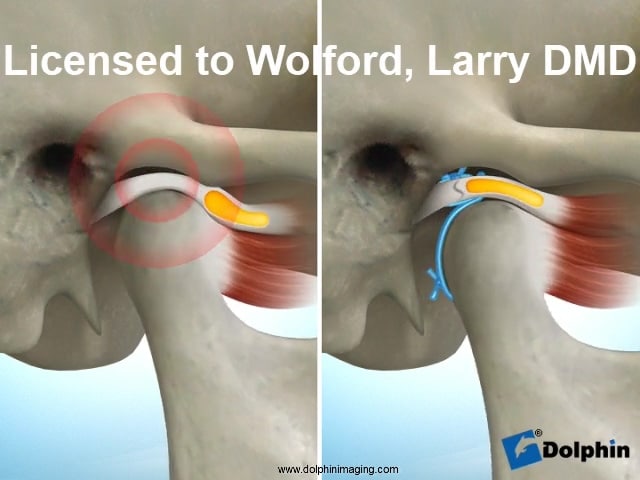
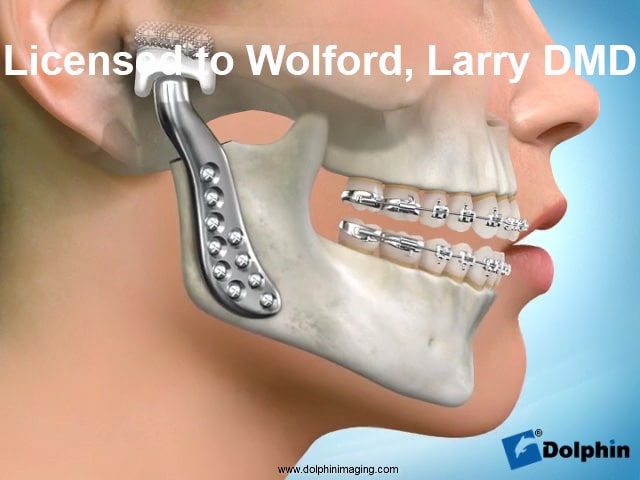
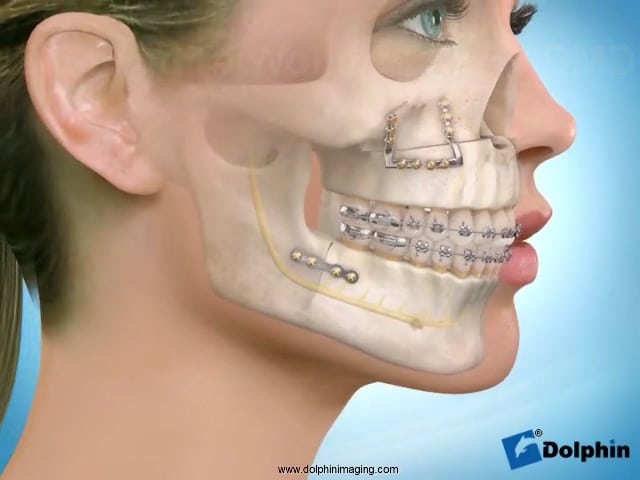
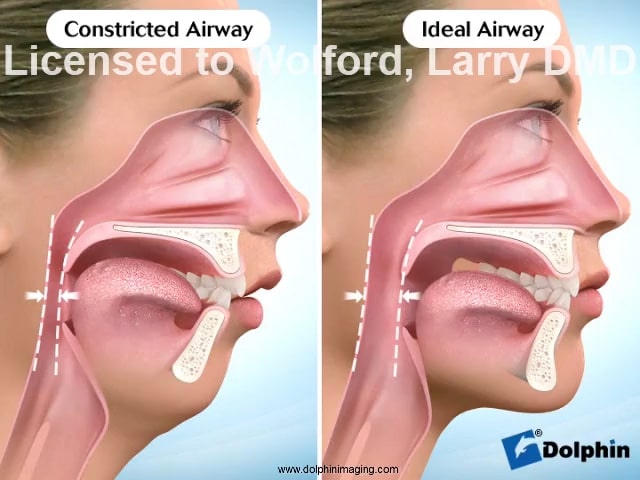
In TMJ joint replacement surgery, the knuckle of the joint has to be cut off and a titanium replacement installed. A little of the bone at the base of the skull is sometimes removed, and replaced with a high-density type of plastic that screws onto the side of the skull. The titanium knuckle sits into the plastic and allows the jaw its full range of movements
When it comes to TMJ replacement surgery, the procedure involves intricate steps to restore proper jaw function. The joint knuckle is carefully removed and replaced with a custom-made titanium implant. In some cases, a portion of the bone at the base of the skull may need to be adjusted and substituted with high-density plastic that attaches securely.
The titanium component fits snugly into the plastic structure, enabling the jaw to regain its complete range of motion. This meticulous process aims to provide patients with improved functionality and relief from debilitating symptoms associated with severe TMJ disorders.
By utilizing advanced materials and techniques, skilled surgeons like Dr. Larry Wolford can effectively address complex jaw issues through precise surgical interventions. TMJ replacement surgery offers hope for individuals facing significant challenges due to damaged temporomandibular joints.
How Long Does The Procedure Take?
The planning and custom manufacture for joint replacement is complex and takes approximately 3 months. This stage begins with the patient undertaking a special very fine slice CT scan which is then used to create draft designs by the implant manufacturer. These designs will be discussed and amended until Dr. Larry Wolford is completely happy that they are perfect.
Following this, a date will be booked at the hospital, and once funding is agreed between the hospital and the insurance company, the 6-week process of the building of the joint can begin. The surgery itself takes approximately 1.5 hours per side. The patient usually remains in hospital as an inpatient for one week and will require some recovery time before returning to work. The patient will be regularly reviewed and patients with chronic pain may require longer admissions.
The journey towards TMJ replacement surgery is a meticulously planned process that spans over several months. It all starts with the patient undergoing a specialized CT scan to kick off the intricate custom manufacturing phase. The implant designs undergo thorough scrutiny and adjustments until perfection, ensuring Dr. Larry Wolford’s satisfaction before moving forward.
Subsequently, after securing hospital booking and funding approval from the insurance company, the actual joint construction takes about six weeks to complete. When it’s time for surgery, each side typically requires around 1.5 hours in the operating room. Following the procedure, patients usually spend a week as inpatients for observation and recovery before resuming their daily routines.
Regular post-surgery check-ups are crucial, especially for patients dealing with chronic pain issues who may need extended hospital stays for proper care and monitoring throughout their healing process.

What Are The Risks of The Procedure?
- As with any joint replacement procedure, one of the main risks is of infection.
- Allergic reaction to implant components.
- Specific to TMJ replacement, risks include facial swelling and facial nerve weakness.
- Heterotopic bone formation (bone found in an abnormal place).
- Neuroma formation (abnormal growth of nerve tissue).
- Ear problems.
- Dislocation.
- Replacement of one joint can cause detrimental effects to the opposite joint.
- Misalignment of the teeth after surgery is possible.
- Patients with long-term pain prior to surgery may continue to experience pain. In this case, the patient will be referred to a chronic pain specialist.
When considering TMJ replacement surgery, it’s crucial to be aware of the potential risks involved. Like any joint replacement procedure, there is a risk of infection that needs to be taken seriously. Additionally, some patients may experience allergic reactions to the implant components used during the surgery.
Specifically related to TMJ replacement, risks can include facial swelling and weakness in the facial nerves post-surgery. Other complications may involve heterotopic bone formation or abnormal growth of nerve tissue known as neuroma formation. Patients should also be mindful of possible ear problems and dislocation following the procedure.
It’s essential to note that replacing one joint can impact the opposite joint negatively and potentially lead to the misalignment of teeth. Furthermore, patients who have experienced long-term pain before surgery may still face challenges afterward, necessitating referral to a chronic pain specialist for ongoing management.
Featured TMJ Videos