Facial trauma can be a life-altering event. Car accidents, sports injuries, falls, and other incidents can cause devastating damage to the intricate structures of the face. Beyond the immediate physical pain, these injuries can profoundly affect a person’s ability to breathe, eat, and speak. They can also impact appearance and self-confidence.
Restoring both function and form after such an injury requires the highly specialized skills of an oral and maxillofacial surgeon. This medical discipline is uniquely positioned at the intersection of dentistry, surgery, and medicine, making its practitioners experts in managing the complexities of the facial skeleton.
This guide explains the types of facial trauma that maxillofacial surgeons treat and highlights why the unparalleled expertise found at Dr. Larry Wolford’s practice is crucial for achieving the best possible outcomes.
What Constitutes Facial Trauma?
Facial trauma refers to any physical injury to the face. Maxillofacial surgeons categorize these injuries based on the type of tissue involved: soft tissue injuries and hard tissue (bone) injuries. Often, a patient will present with a combination of both.
1. Soft Tissue Injuries
These injuries involve the skin and underlying muscles of the face and neck. They include:
- Lacerations: Cuts or tears in the skin.
- Abrasions: Scrapes that damage the outer layers of skin.
- Contusions: Bruises caused by blunt force trauma.
While some minor lacerations can be treated in an emergency room, complex facial cuts require a surgeon’s touch. A maxillofacial surgeon meticulously sutures these wounds layer by layer to minimize scarring and prevent damage to underlying nerves and glands, such as salivary glands and ducts.
2. Hard Tissue Injuries (Facial Fractures)
Fractures of the facial bones are the most serious form of facial trauma. The goal of treatment is to return the bones to their original position and stabilize them so they can heal properly. This restores the patient’s facial structure and function. Common facial fractures include:
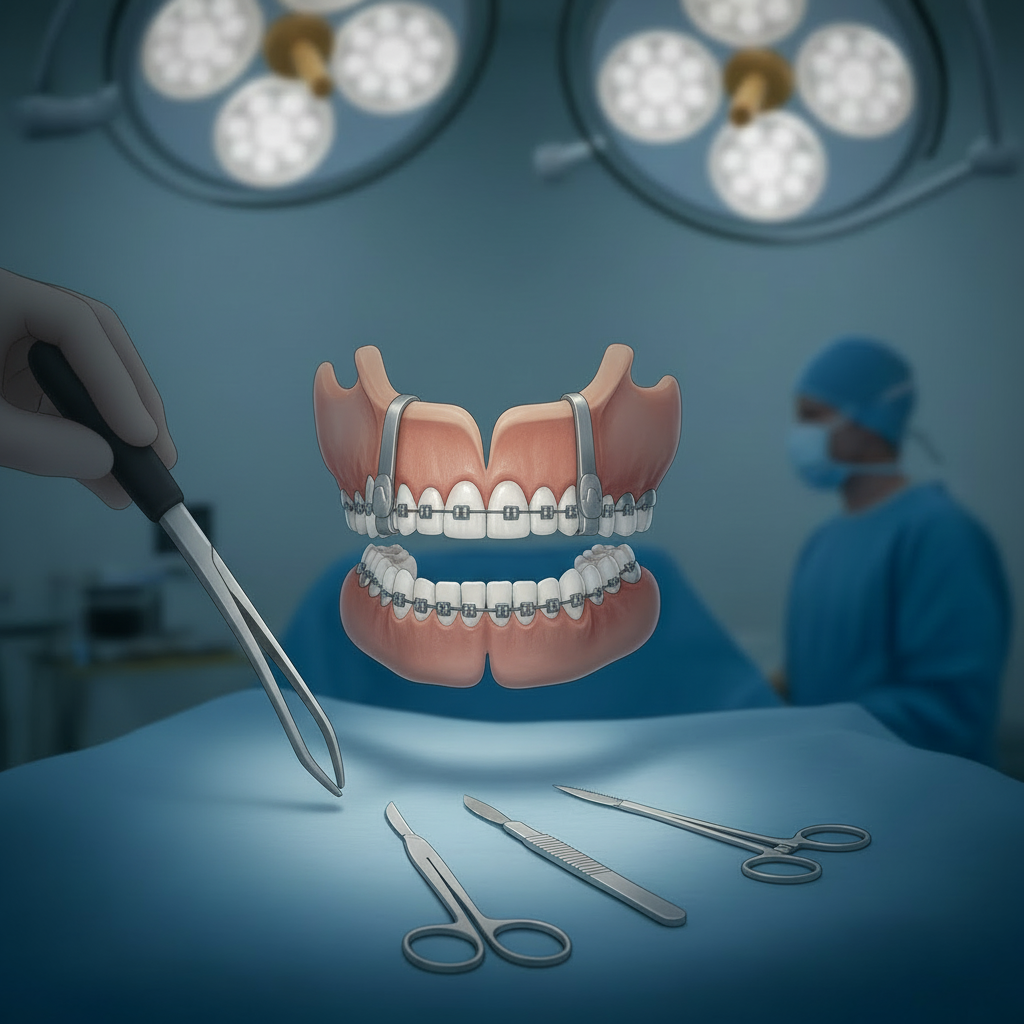
- Mandibular Fractures (Lower Jaw): A broken lower jaw can affect your bite and ability to open your mouth. Treatment often involves wiring the jaws shut or surgically placing small plates and screws to hold the bone fragments together—a technique called rigid fixation.
- Maxillary Fractures (Upper Jaw): A fracture of the upper jaw can affect breathing, vision, and the alignment of the teeth. These are often classified using the Le Fort system (I, II, and III) based on the fracture pattern.
- Zygomatic Fractures (Cheekbone): A broken cheekbone can result in a flattened appearance and may impinge on the jaw’s movement.
- Orbital Fractures (Eye Socket): Fractures of the delicate bones around the eye can cause double vision, a sunken eye appearance, and nerve damage. Repairing these requires extreme precision to protect the eye and its associated nerves and muscles.
The American Association of Oral and Maxillofacial Surgeons (AAOMS) emphasizes that these surgeons are extensively trained in the emergency care, acute treatment, and long-term reconstruction of facial trauma patients.
The Maxillofacial Surgeon’s Approach to Treatment
Treating facial trauma is a meticulous process that balances immediate needs with long-term functional and aesthetic goals.
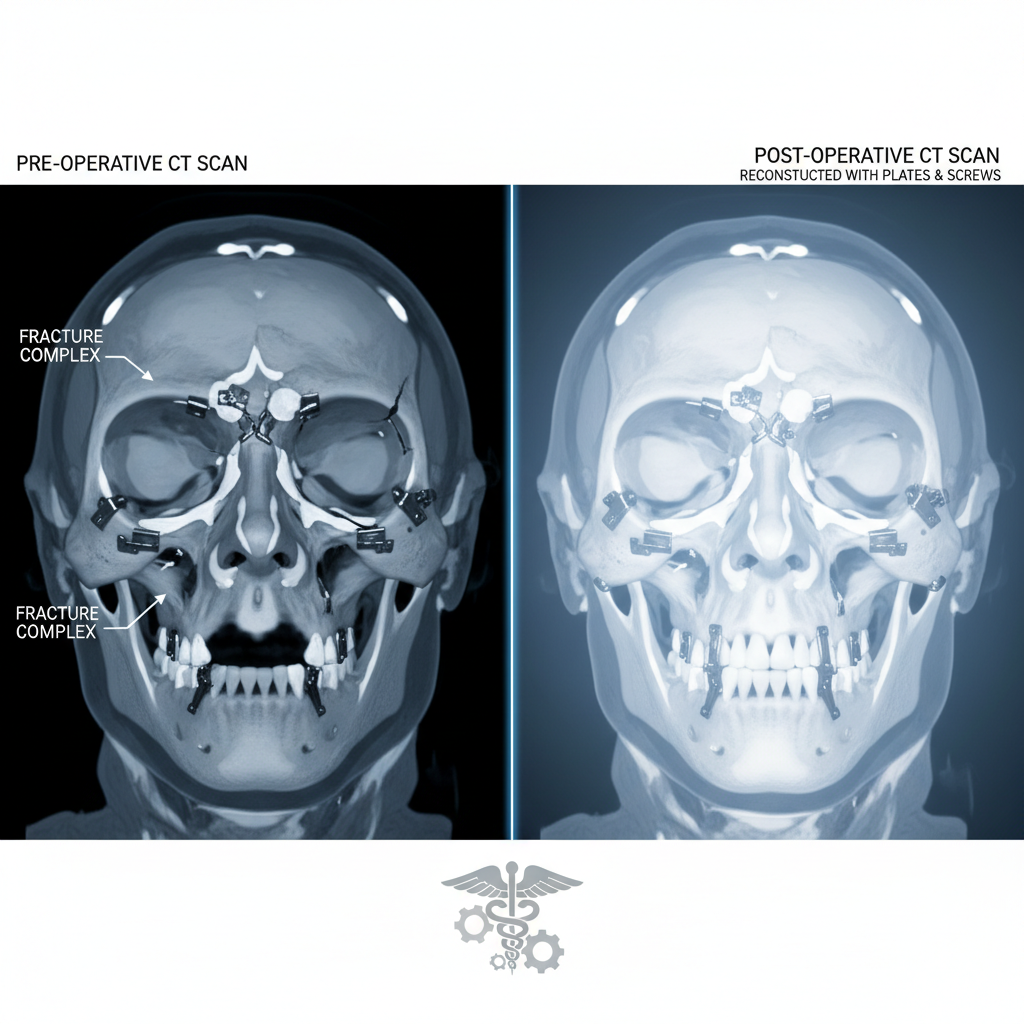
Step 1: Diagnosis and Planning
The first step is a comprehensive evaluation. Advanced imaging, such as CT scans, is used to create a detailed 3D map of the facial skeleton. This allows the surgeon to precisely identify the location and severity of all fractures. This digital blueprint is essential for planning the surgical approach.
Step 2: Surgical Repair
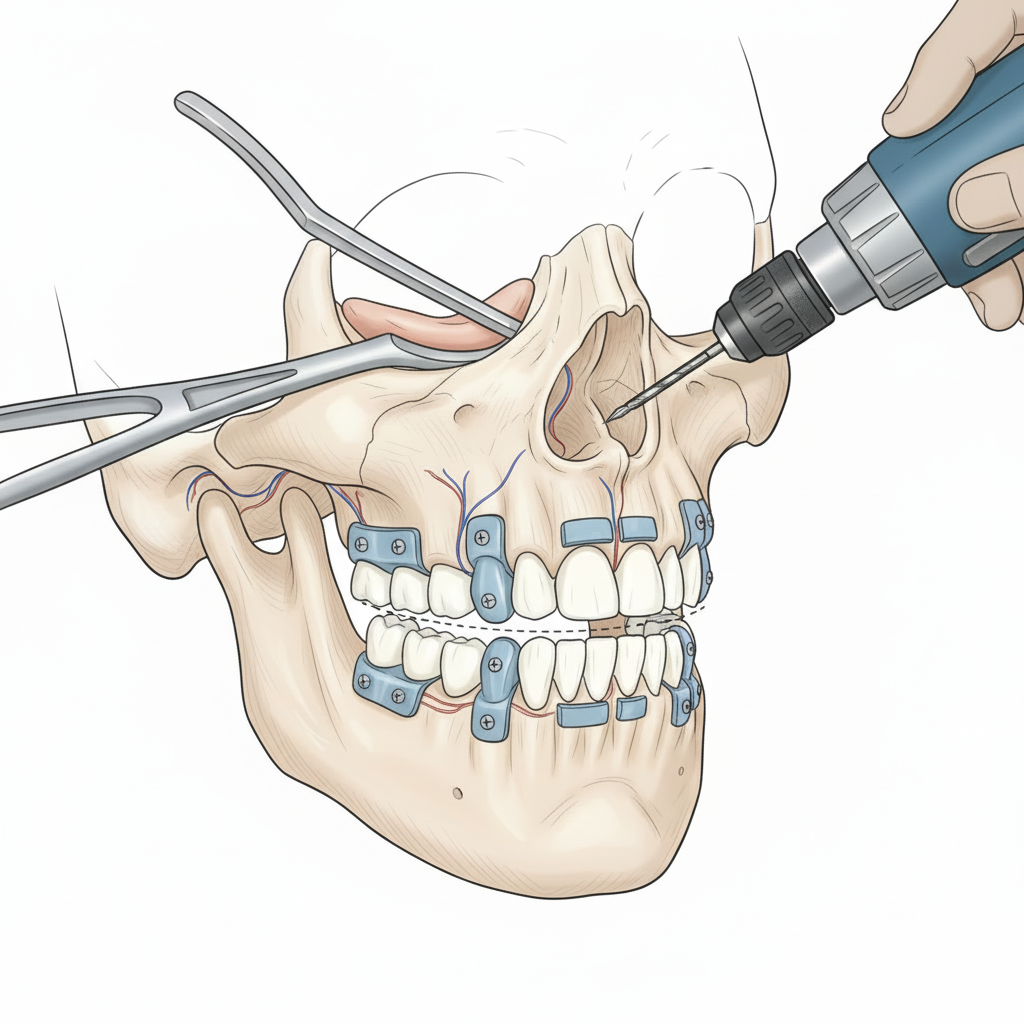
The primary principle of facial fracture repair is “reduction and fixation.”
- Reduction: The fractured bone fragments are carefully moved back into their correct anatomical position.
- Fixation: The reduced fragments are held in place using medical-grade titanium plates and screws. This rigid internal fixation provides stability, allowing the bones to heal without the need for prolonged periods of having the jaw wired shut.
Surgery is often performed through incisions made inside the mouth or along natural skin creases to minimize visible scarring. The surgeon’s deep understanding of facial anatomy is critical to avoid damaging nerves, blood vessels, and tear ducts.
Step 3: Long-Term Reconstruction
In severe cases, the initial trauma may result in bone or tissue loss. Long-term reconstruction might be necessary, which can involve bone grafting to replace missing segments of the jaw or orbital floor. The surgeon’s goal is always to restore the patient’s pre-injury appearance and function as closely as possible.
Why Specialized Expertise Is Non-Negotiable: The Dr. Wolford Standard
The face is arguably the most complex anatomical region of the body. Successful reconstruction depends not just on technical skill but on a profound understanding of facial aesthetics and biomechanics.
Dr. Larry Wolford is a world-renowned expert in facial reconstruction, particularly for patients with complex and revision trauma cases. His practice is a destination for patients whose initial treatments elsewhere were unsuccessful or led to complications.
Dr. Wolford’s expertise provides several key advantages:
- Comprehensive Skillset: As a leader in both TMJ and orthognathic surgery, Dr. Wolford possesses an unmatched understanding of how the jaws, joints, and facial bones work together. This holistic view is critical when trauma affects multiple structures.
- Advanced Surgical Planning: Utilizing state-of-the-art 3D virtual surgical planning, Dr. Wolford can digitally perform the surgery before entering the operating room. This allows for unparalleled precision, predictable outcomes, and the creation of custom-fit surgical plates if needed.
- Focus on Function: Restoring a patient’s bite (occlusion) is a top priority. Dr. Wolford ensures that once the bones heal, the teeth will meet correctly, allowing for proper chewing and speaking. This integration of dental and surgical principles is a hallmark of the specialty.
For in-depth research on surgical techniques in this field, the Journal of Oral and Maxillofacial Surgery provides extensive, peer-reviewed articles on facial trauma management.
Beyond the Operating Room
Recovery from facial trauma surgery depends on the extent of the injuries. It often involves a period of soft diet, limited physical activity, and follow-up appointments to monitor healing. The titanium plates and screws are biocompatible and typically remain in place for life without causing issues.
The ultimate goal of maxillofacial trauma surgery is to make the traumatic event a memory, not a permanent fixture of the patient’s life. By restoring the intricate architecture of the face, surgeons help patients regain their health, function, and identity.
Navigating Your Path to Recovery
If you or a loved one has suffered a facial injury, seeking care from a qualified oral and maxillofacial surgeon is the most important step you can take. For complex cases, revision surgery, or when the highest level of expertise is required, Dr. Larry Wolford’s practice offers definitive solutions.
Contact our office today to schedule a comprehensive consultation. Let our team provide the expert care needed to restore your health and confidence.