The field of maxillofacial surgery, dedicated to treating the complex anatomy of the face, jaw, and mouth, has always been at the forefront of medical advancement. From pioneering techniques developed during wartime to the adoption of rigid fixation for fractures, its history is one of continuous improvement. Today, we are witnessing another profound transformation, one driven by the powerful integration of digital technology into every stage of patient care.
Advanced technologies like artificial intelligence (AI), surgical robotics, and 3D printing are no longer concepts from science fiction; they are becoming integral tools in the modern surgical suite. This convergence of medicine and technology is revolutionizing maxillofacial surgery, leading to unprecedented levels of precision, predictability, and personalization. For patients, this means safer procedures, quicker recoveries, and better functional and aesthetic outcomes. This article explores these groundbreaking innovations and how they are shaping the future of facial reconstruction and care.
Virtual Surgical Planning: The Digital Blueprint for Success
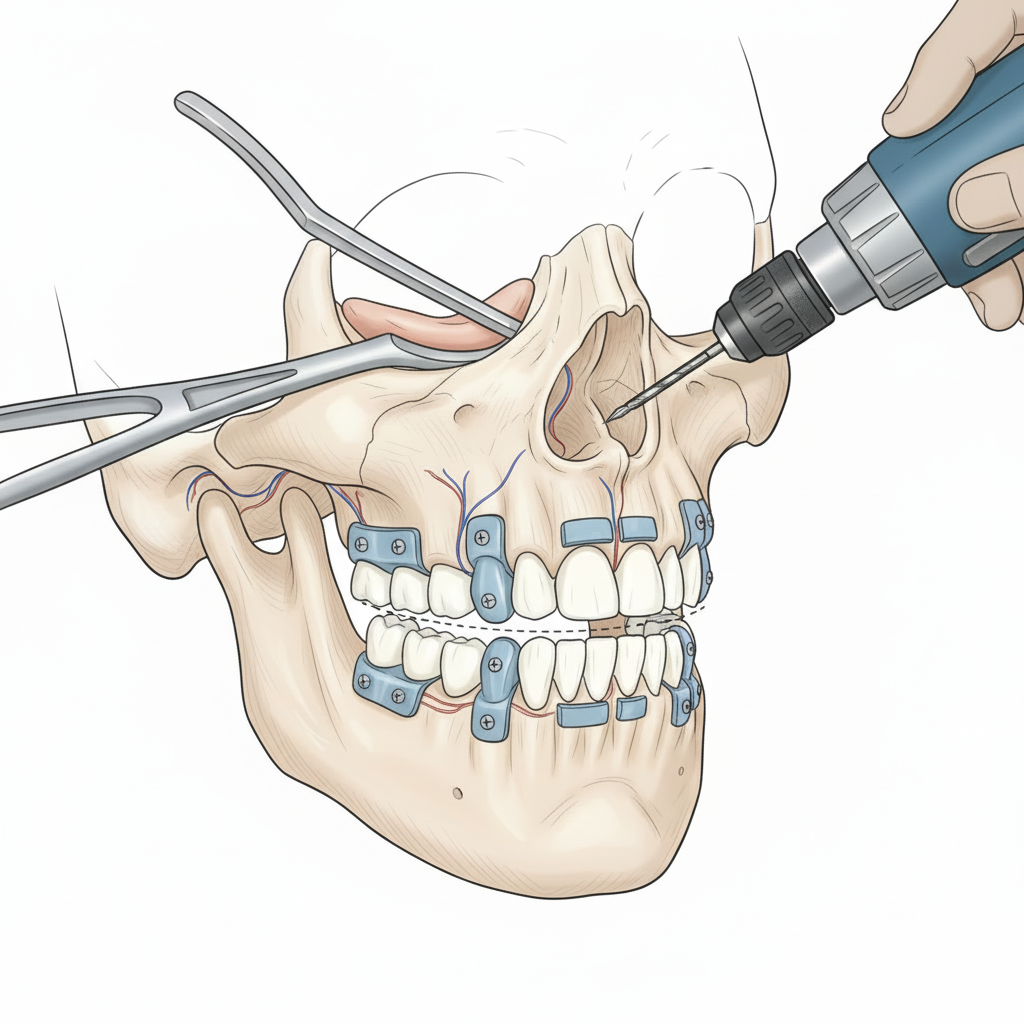
Perhaps the most significant innovation in recent years is the widespread adoption of Virtual Surgical Planning (VSP). Before VSP, surgeons relied on 2D X-rays and physical models to plan complex procedures. Now, with Cone Beam Computed Tomography (CBCT) scans, they can create a perfect digital replica of a patient’s skull (NCBI – 3D Imaging in Maxillofacial Surgery).
Using specialized software, a surgeon can perform the entire operation in a virtual environment before ever stepping into the operating room. This digital rehearsal allows for sub-millimeter precision in planning bone cuts, repositioning jaw segments, and predicting the final outcome. The benefits are immense:
- Enhanced Precision: Surgeons can plan the exact movements needed to achieve the best functional and aesthetic result, minimizing surprises during the actual procedure.
- Reduced Operating Time: A detailed pre-operative plan translates to more efficiency in the operating room, which can reduce anesthesia time and lower risks.
- Predictable Outcomes: VSP allows both the surgeon and patient to see a simulation of the post-surgical result, helping to align expectations and refine the treatment plan.
This technology is central to modern orthognathic (corrective jaw) surgery, facial trauma repair, and complex reconstructive procedures (AAOMS – Surgical Planning Technologies).
3D Printing: From Custom Guides to Patient-Specific Implants
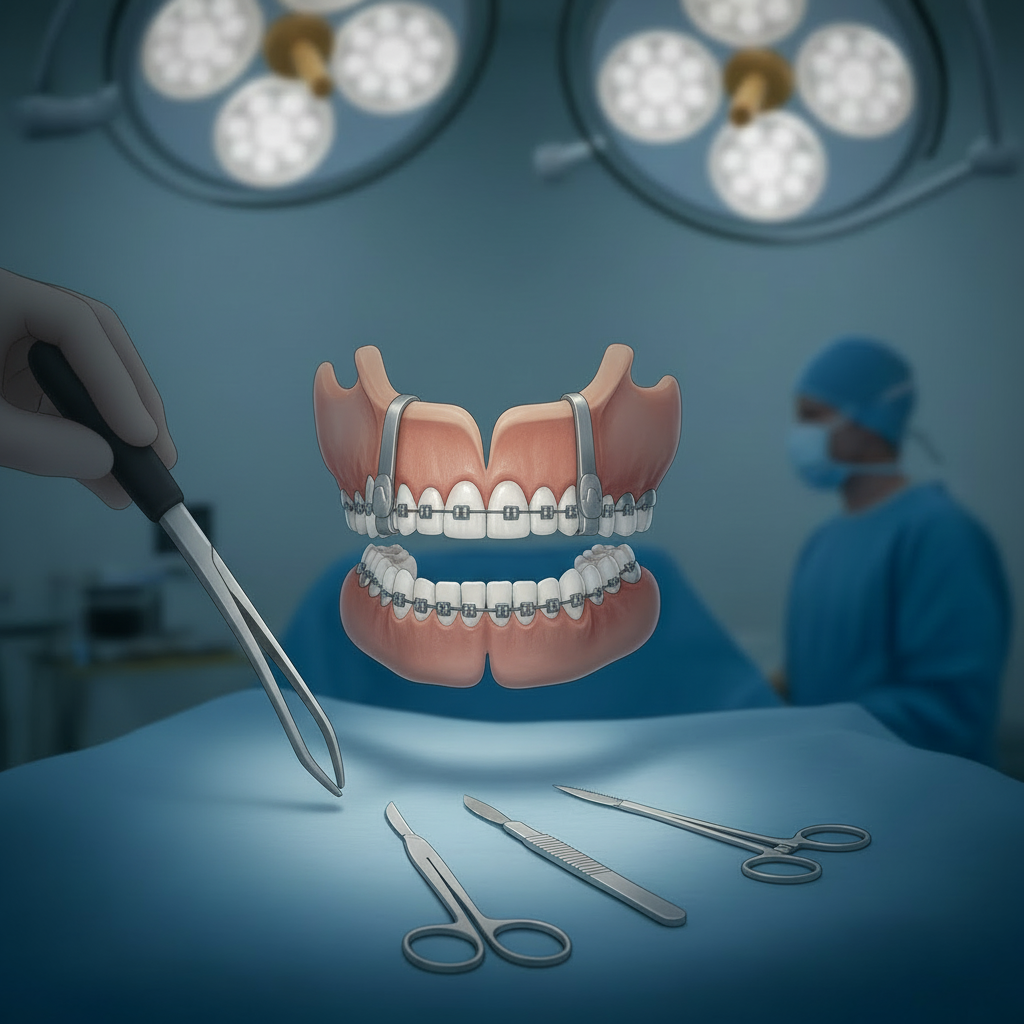
Working hand-in-hand with VSP, 3D printing has moved from a novelty to a critical manufacturing tool in maxillofacial surgery. Its applications are varied and transformative.
Surgical Guides
Once a virtual plan is finalized, the surgeon can 3D print custom surgical guides. These guides are sterilized and placed directly on the patient’s bone during surgery, fitting perfectly onto their unique anatomy (Journal of Oral and Maxillofacial Surgery – 3D-Printed Surgical Guides). They contain precise slots that direct the saw blade, ensuring the bone cuts are executed exactly as planned in the virtual model. This technology bridges the gap between the digital plan and the physical reality of the operating room.
Patient-Specific Implants
For patients with significant bone loss from trauma, congenital defects, or tumor removal, off-the-shelf implants may not provide an ideal fit. A Maxillofacial Surgeon can now use a patient’s CT scan to design and 3D print an implant that is a perfect mirror image of their own anatomy. These patient-specific implants, often made from biocompatible materials like titanium or PEEK, offer superior fit, function, and aesthetics (Nature – Patient-Specific Implants). This is especially critical in total temporomandibular joint (TMJ) replacements, where a custom fit is essential for restoring natural jaw movement.
AI and Robotics: The Next Frontier of Precision
The next wave of innovation is being driven by artificial intelligence and robotics, promising to enhance the surgeon’s capabilities even further.
AI in Diagnostics and Planning
AI algorithms are being developed to analyze medical images with a level of detail that can surpass the human eye (Frontiers in Surgery – AI in Maxillofacial Imaging). These systems can help identify pathologies, segment anatomical structures, and even suggest an optimal surgical plan based on data from thousands of successful cases. AI can also create highly accurate simulations of how a patient’s facial soft tissues will drape over the newly positioned bones, providing a more reliable preview of the final appearance (NCBI – AI and Simulation in Surgery).
Robotics in the Operating Room
Surgical robots, known for their stability and dexterity, are beginning to find a place in maxillofacial procedures. A robotic arm, guided by the VSP, could potentially execute bone cuts or place screws with unwavering precision (Journal of Dental Research – Robotics in OMS). This technology is particularly promising for minimally invasive procedures, allowing surgeons to work through small incisions with magnified 3D vision. While still emerging, robotic assistance has the potential to make delicate surgeries safer and more consistent.
Augmented Reality (AR) is another technology set to enhance the surgeon’s view. By wearing AR glasses, a surgeon could see the 3D surgical plan, including the location of nerves and blood vessels, projected directly onto the patient (International Journal of Oral and Maxillofacial Surgery – AR in Surgery). This real-time guidance system acts as a digital map, further improving accuracy and safety.
Tissue Engineering: Regenerating, Not Just Replacing
One of the most exciting areas of innovation is regenerative medicine. The ultimate goal is to help the body regrow its own lost or damaged tissue. In maxillofacial surgery, this is becoming a reality through tissue engineering (NIH – Tissue Engineering in Maxillofacial Surgery).
Instead of harvesting bone from a patient’s hip or leg to reconstruct the jaw—a process that involves a second surgical site and significant discomfort—surgeons are using advanced biologics. Bone Morphogenetic Proteins (BMPs) are signaling molecules that can be placed in a surgical site to recruit the body’s own stem cells and instruct them to form new bone (U.S. National Library of Medicine – BMPs in Oral Surgery). This technology can reduce the need for traditional bone grafts, leading to faster and less painful recoveries.
Researchers are also working on 3D-printed biodegradable scaffolds. These can be printed in the exact shape of the missing bone and implanted. As the body grows new bone tissue throughout the scaffold, the scaffold itself slowly dissolves, leaving behind only the patient’s natural, living bone (ScienceDirect – 3D-Printed Scaffolds in Bone Regeneration).
The Surgeon’s Role in a High-Tech World
With all these technological advancements, the role of the maxillofacial surgeon becomes more important, not less. The surgeon is the master conductor, orchestrating these complex technologies to benefit the patient. Their deep understanding of anatomy, biology, and surgical principles is essential to create the virtual plan, guide the technology, and make critical decisions during the procedure (AAOMS – About Oral and Maxillofacial Surgeons).
Adopting these innovations requires a commitment to lifelong learning and the ability to critically evaluate which technologies truly add value to patient care. The surgeon’s expertise ensures that these powerful tools are used safely, effectively, and for the right indications, translating technological potential into real-world healing. The future is not about technology replacing the surgeon, but about technology empowering the surgeon to achieve what was previously impossible.