Maxillofacial surgery has undergone a remarkable transformation over the last few decades, moving from traditional open procedures to highly precise, digitally planned interventions. The integration of 3D imaging and virtual surgical planning has already set a new standard of care, offering patients better outcomes and faster recoveries (AAOMS: Virtual Surgical Planning). But this field, which lies at the intersection of medicine, dentistry, and technology, is not standing still. The next wave of innovation is poised to make treatment even more precise, less invasive, and highly personalized.
Looking ahead, we can see a future where robotics enhance surgical precision, damaged tissues are regrown rather than replaced, and artificial intelligence helps predict outcomes with incredible accuracy. These emerging trends are set to redefine the boundaries of what is possible in treating conditions of the face, mouth, and jaw. This article explores the exciting future of maxillofacial surgery and the technologies that will shape it.
AI and Machine Learning in Surgical Planning
While virtual surgical planning (VSP) is already a game-changer, artificial intelligence (AI) and machine learning are set to make it even more powerful (Frontiers in Artificial Intelligence: Applications in Surgery). Currently, a surgeon manually manipulates a 3D model to plan a procedure. In the future, AI algorithms will be able to analyze a patient’s CT scan and suggest an ideal surgical plan based on thousands of previous cases and established aesthetic and functional principles.
This technology could:
- Predict Outcomes: AI models can simulate how a patient’s soft tissues will respond to underlying skeletal changes, providing a more accurate preview of the final aesthetic result (Nature: AI in Craniofacial Imaging and Diagnosis). This helps manage patient expectations and allows for finer adjustments before surgery.
- Optimize Treatment: Machine learning can identify subtle patterns and correlations that are invisible to the human eye, potentially suggesting more efficient surgical movements or flagging potential risks (NCBI: Machine Learning and Surgery).
- Automate Planning: AI could automate the more repetitive aspects of surgical planning, freeing up the Maxillofacial Surgeon to focus on the most critical and nuanced decisions. This efficiency could make advanced surgical planning more accessible and standardized.
Robotics and Augmented Reality in the Operating Room
Robotics have already made a significant impact in fields like urology and general surgery, and their adoption in maxillofacial surgery is on the horizon (Journal of Oral and Maxillofacial Surgery: Robotic Surgery). Surgical robots offer enhanced dexterity, tremor filtration, and magnified 3D vision, allowing surgeons to perform incredibly delicate tasks with greater precision.
In maxillofacial surgery, robotics could be used for:
- Precise Bone Cuts: A robotic arm, guided by the pre-operative virtual plan, could execute bone cuts with sub-millimeter accuracy, surpassing what is possible by human hands alone (Robotics and Computer-Assisted Surgery in OMS).
- Minimally Invasive Procedures: Robots can operate through smaller incisions, which is particularly beneficial for procedures like TMJ arthroscopy or accessing difficult-to-reach tumors.
Complementing robotics is Augmented Reality (AR). Imagine a surgeon wearing AR glasses that overlay the 3D surgical plan directly onto the patient in the operating room. This would provide real-time guidance, allowing the surgeon to see the exact location of critical nerves and blood vessels and verify that the surgical movements match the plan perfectly (JMIR: Augmented Reality in Surgery). This fusion of the digital plan with the physical reality promises to enhance safety and accuracy.
Tissue Engineering and Regenerative Medicine
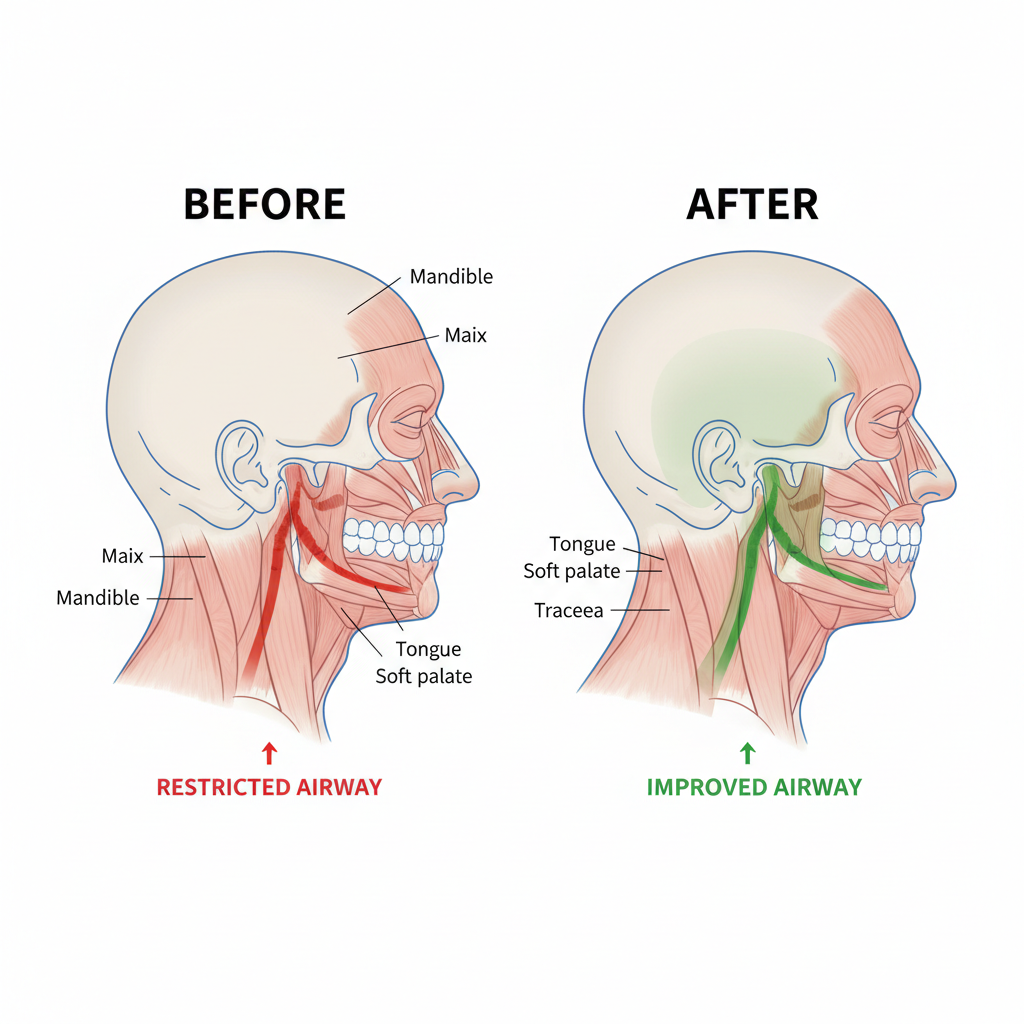
One of the most exciting frontiers in maxillofacial surgery is the shift from reconstruction to regeneration. Currently, when bone or tissue is missing due to trauma or disease, it is often replaced with bone grafts from other parts of the body or with synthetic implants. Tissue engineering aims to persuade the body to regrow its own lost tissue (NIH: Tissue Engineering of Bone).
Key advancements in this area include:
- Bone Morphogenetic Proteins (BMPs): These are growth factors that can be applied to a surgical site to stimulate the body’s own stem cells to form new bone (AAOMS: Bone Morphogenetic Proteins). Their use is already reducing the need for extensive bone harvesting, which means less pain and a faster recovery for the patient.
- 3D-Printed Scaffolds: Researchers are developing biocompatible, biodegradable scaffolds that can be 3D-printed in the exact shape of the missing bone (ScienceDirect: 3D Printed Scaffolds for Bone Repair). These scaffolds provide a template for new bone cells to grow on. As the new bone forms, the scaffold gradually dissolves, leaving behind natural, living tissue.
- Growing Cartilage: For complex TMJ disorders, regenerating the disc of cartilage within the joint is a major goal. Ongoing research is focused on using a patient’s own cells to grow new cartilage in a lab, which could then be implanted to restore joint function (International Journal of Oral Science: TMJ Tissue Engineering). Major research institutions are actively exploring methods to make this a clinical reality.
Customization and Patient-Specific Implants
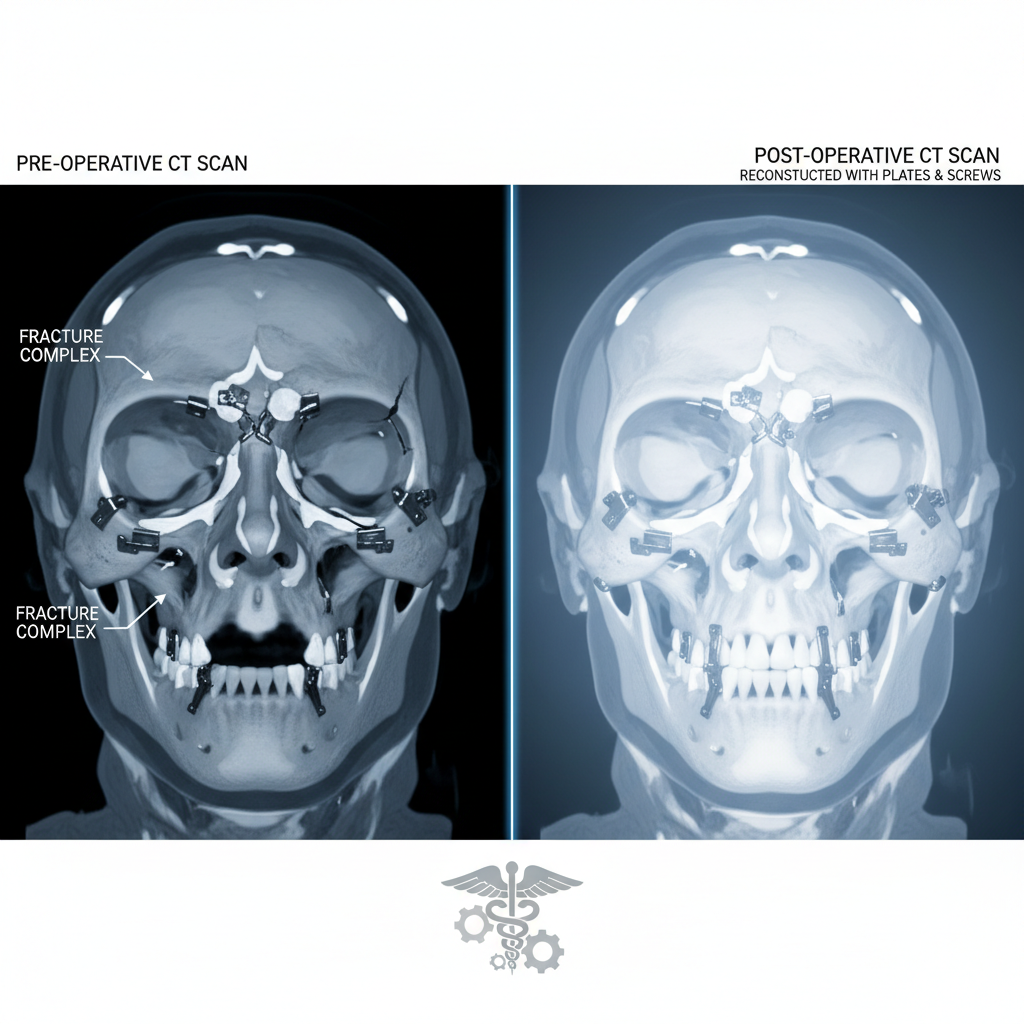
The “one-size-fits-all” approach to medical devices is rapidly becoming obsolete. Thanks to 3D printing, the future of maxillofacial surgery is entirely custom (Journal of Oral Biology and Craniofacial Research: 3D Printing in Surgery). We have already seen the benefits of patient-specific implants for total jaw joint replacements and complex trauma reconstruction. This trend is set to expand dramatically.
In the near future, nearly every implant—from the plates and screws used in orthognathic surgery to the dental implants themselves—could be custom-manufactured for each individual. These patient-specific implants offer several advantages:
- Perfect Fit: A custom implant fits the patient’s anatomy precisely, reducing surgery time and improving stability.
- Better Functional Outcomes: Implants designed for the individual’s specific biomechanical needs can lead to better long-term function (Journal of Cranio-Maxillofacial Surgery: Patient-Specific Implants).
- Improved Aesthetics: In facial reconstruction, custom implants allow for a more accurate restoration of the patient’s original appearance.
Advancements in Anesthesia and Pain Management
Patient safety and comfort remain a top priority. Future advancements will focus on making recovery from maxillofacial surgery faster and less painful. This includes the development of longer-acting local anesthetics that can provide pain relief for days after surgery, reducing the need for opioid medications (NIH: Advances in Pain Management).
Furthermore, refined anesthesia protocols and non-invasive monitoring will continue to make complex, lengthy procedures safer for patients with all types of health profiles. The expertise of maxillofacial surgeons in anesthesia administration will be crucial in implementing these new techniques (AAOMS: Office-based Anesthesia).
A New Era of Restoration and Healing
The future of maxillofacial surgery is exceptionally bright. The convergence of AI, robotics, tissue engineering, and digital manufacturing is paving the way for a new era of personalized, predictive, and regenerative medicine. These innovations will empower surgeons to restore both form and function with an unprecedented level of precision and success. For patients, this means safer procedures, faster recoveries, and outcomes that were once considered the stuff of science fiction. The core mission remains the same—to improve lives—but the tools to achieve it are becoming more powerful every day.