TLDR: A Guide to Craniofacial Deformities
- Craniofacial deformities affect the growth and development of the head and face (e.g., cleft lip/palate, craniosynostosis).
- Causes can include genetic factors, environmental influences, or may be unknown.
- Early diagnosis is vital to ensure the best outcomes for children and families.
- Multidisciplinary care teams (surgeons, pediatricians, therapists, etc.) provide comprehensive and coordinated support.
- Advances in treatment—including innovative surgeries and non-surgical therapies—offer improved results.
- Families can find support, resources, and financial aid through dedicated organizations and community networks.
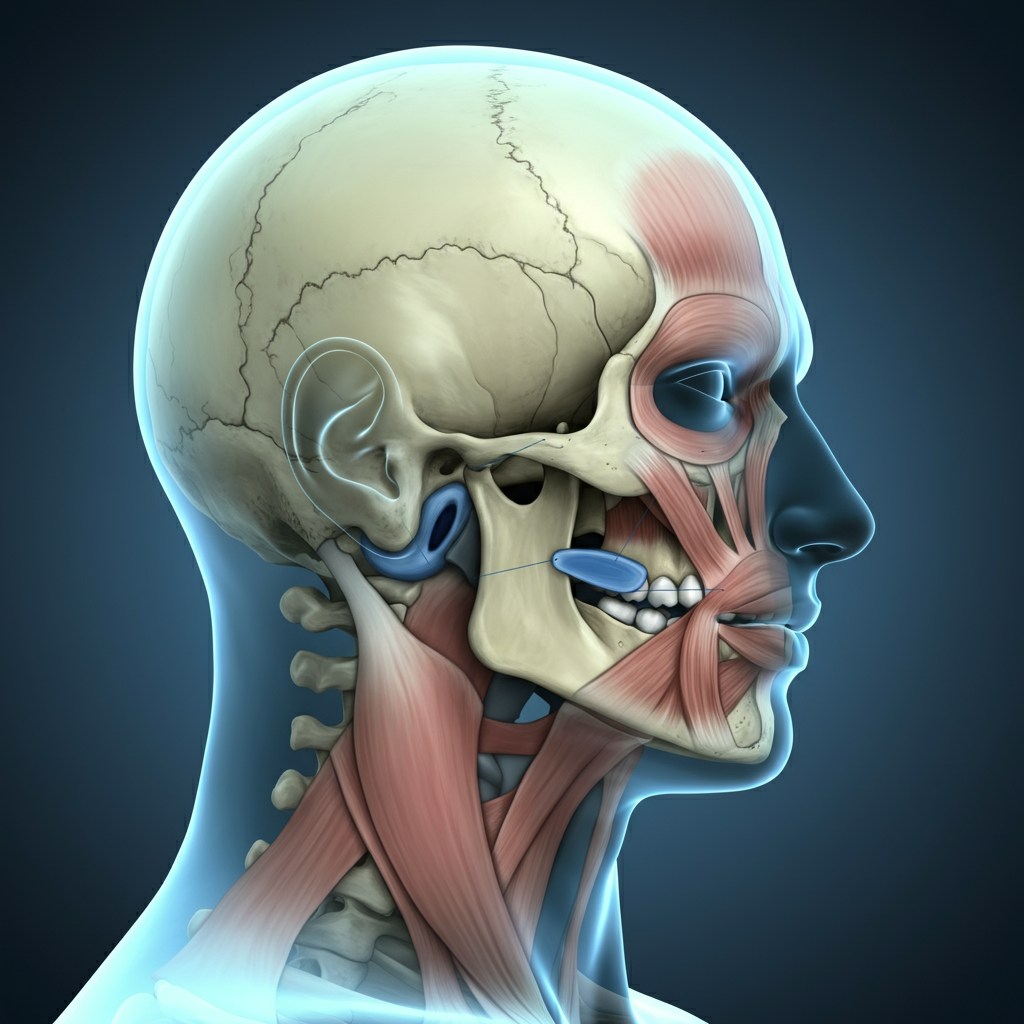
Receiving a diagnosis of a craniofacial deformity for your child, or navigating this journey as an individual, can feel overwhelming. These conditions, which affect the bones and soft tissues of the head and face, present unique challenges. However, understanding the condition is the first step toward accessing incredible systems of support and advanced medical care. This guide offers a compassionate overview of craniofacial deformities, from common types to the comprehensive care available today.
What Are Craniofacial Deformities?
Craniofacial deformities are a diverse group of conditions resulting from abnormal growth and development of the head and facial structures. These conditions can range from mild to severe and may be present at birth (congenital) or develop later due to injury or disease.
The causes are often complex and can include a combination of factors:
- Genetic Factors: Many conditions are linked to specific gene mutations that can be inherited or occur spontaneously.
- Environmental Influences: Certain factors during pregnancy, such as exposure to specific medications or infections, may play a role.
- Unknown Causes: In many cases, the exact cause remains unknown.
It’s important to remember that this is not the result of anything a parent did or did not do. The focus should always be on support and finding the best path forward.
Common Types of Craniofacial Conditions
While there are hundreds of different craniofacial conditions, some are more common than others.
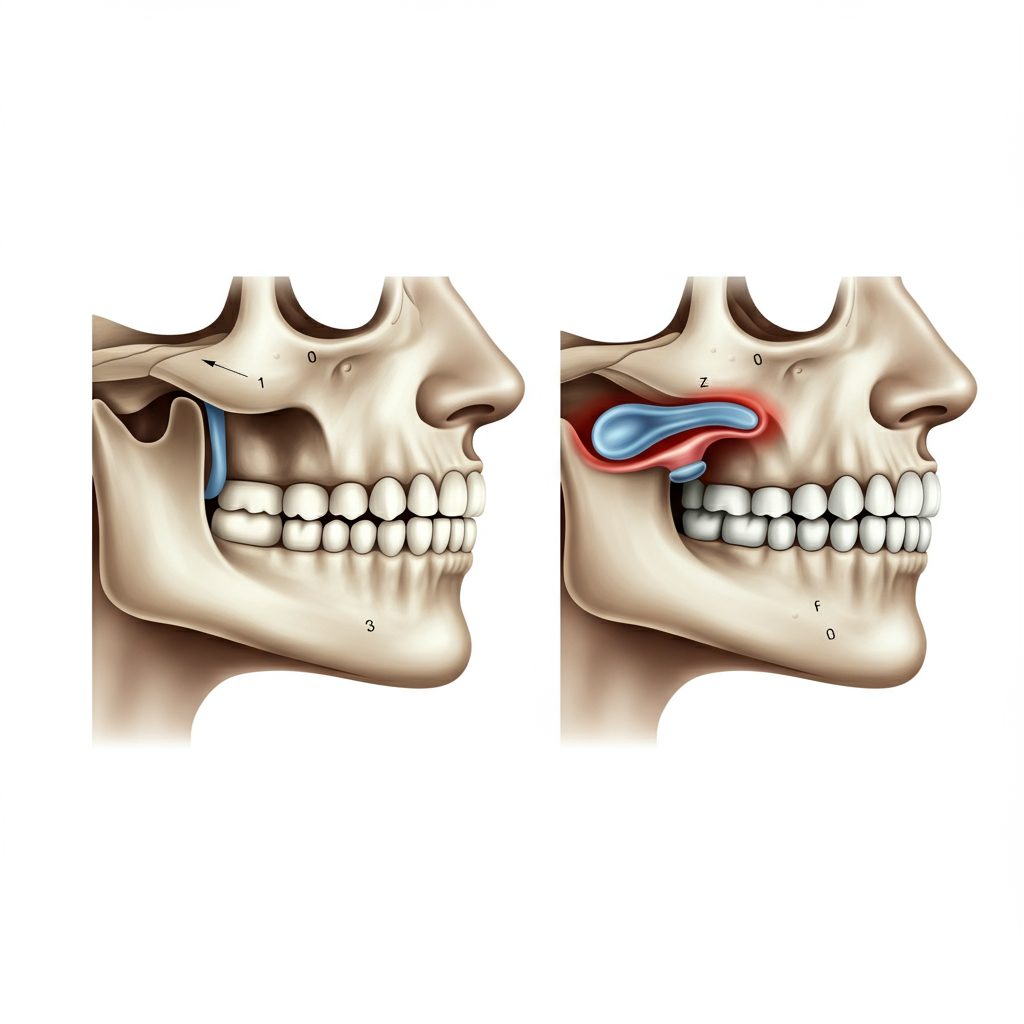
- Cleft Lip and Cleft Palate: One of the most well-known conditions, a cleft lip is a physical split or separation of the two sides of the upper lip. A cleft palate is a split in the roof of the mouth. These occur when facial structures developing in an unborn baby don’t close completely. They can impact feeding, speech, and hearing.
- Craniosynostosis: This condition involves the premature fusion of one or more of the flexible seams (sutures) in an infant’s skull. As the brain grows, this early fusion can cause the skull to grow into an abnormal shape and, in some cases, lead to increased pressure on the brain.
- Hemifacial Microsomia: This condition affects the development of the lower half of one side of the face, including the ear, mouth, and jaw. The severity can vary greatly, from nearly unnoticeable to significant facial asymmetry.
The Importance of Early Diagnosis and Multidisciplinary Care
Early diagnosis is key to developing an effective treatment plan and ensuring the best possible outcome. Often, a diagnosis is made during prenatal ultrasounds or shortly after birth. This allows families to connect with specialists right away.
Treating craniofacial conditions is a team effort. A multidisciplinary care team brings together experts from various fields to provide comprehensive, coordinated care. Your team may include:
- Craniofacial Surgeons: Plastic and reconstructive surgeons who specialize in the skull and face.
- Pediatricians: To manage overall health and development.
- Orthodontists and Dentists: To address dental and jaw alignment.
- Speech-Language Pathologists: To help with feeding and speech development.
- Otolaryngologists (ENTs): To manage hearing and breathing issues.
- Geneticists: To help identify underlying causes and provide counseling.
- Psychologists and Social Workers: To provide emotional support for the individual and family.
This team-based approach ensures that every aspect of a child’s health and well-being is addressed throughout their journey.
Advancements in Treatment
The field of craniofacial medicine has made remarkable progress. Treatment is highly individualized and depends on the specific condition and its severity.
- Surgical Treatments: Surgery is often a cornerstone of treatment. For a cleft lip, surgery is typically performed in the first few months of life, while palate repair often happens within the first year. For craniosynostosis, surgery can relieve pressure on the brain and correct the skull’s shape. Surgeons now use advanced techniques, including minimally invasive procedures and 3D modeling, to plan and execute complex operations with greater precision.
- Non-Surgical Treatments: Many aspects of care are non-surgical. Orthodontic devices can help align the jaw and teeth before or after surgery. Molding helmets can be used to gently reshape the skull in some infants with positional plagiocephaly (flat head syndrome) or after certain types of craniosynostosis surgery. Speech therapy is crucial for children with cleft palates to develop clear communication skills.
Finding Support and Resources
You are not alone on this journey. Connecting with other families who have similar experiences can provide invaluable emotional support and practical advice. Many organizations offer resources, information, and a sense of community.
Consider reaching out to these reputable organizations for further support:
- Children’s Craniofacial Association (CCA): Provides financial assistance for travel to specialized medical centers and connects families through a network of support.
- FACES: The National Craniofacial Association: Offers financial support for travel expenses related to medical care and raises public awareness.
- myFace: Delivers comprehensive care and support by funding medical, dental, speech, and psychosocial services.
Navigating a craniofacial diagnosis requires courage and resilience. With dedicated medical teams, evolving treatments, and strong support networks, individuals with these conditions can thrive and lead full, healthy lives.